Iris Cysts
By Paul T. Finger, MD
Description
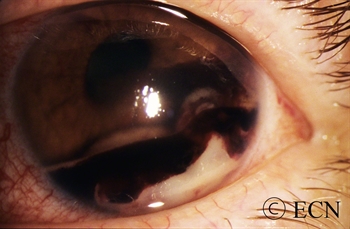
Cysts can form in different parts of the iris and ciliary body. Most remain undetected, unless they push on the iris or get relatively large. The most common is the neuro-epithelial iris cyst, which is typically located beneath the iris root. Cysts can also be located in the ciliary body, the iris stroma, and be formed by splitting (schisis) of the iris pigment epithelium). These cysts can push the iris forward, appear as a mass or tumor and may cause angle closure glaucoma.
Symptoms
Almost all iris cysts are located behind the iris and cause no symptoms. They are found by the eye care specialist during ophthalmic examination. Iris stromal cysts can become visible on the surface of the iris. Most commonly, the eye doctor sees a bulge in the iris stroma and considers that a tumor may be pushing it forward. At that point, the doctor may send the patient for an ocular tumor evaluation (to look behind the iris with ultrasound or OCT imaging).
Diagnosis
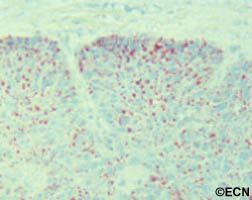
Most iris cysts can be diagnosed by clinical examination with high-frequency ultrasonography.
Large cysts can be seen by routine slit-lamp examination.
Though cysts are benign, periodic observation is necessary due to the rare instances of secondary angle closure glaucoma (only seen with giant cysts, multifocal cysts and iris schisis cysts).

High-frequency ultrasonography (aka UBM) has revolutionized our ability to image and thus “see” tissues behind the iris. It has allowed for evaluation of tumor thickness, depth of penetration, and invasion of adjacent tissues. Ultrasounds ability to determine if a tumor is solid or cystic has been particularly helpful.
Treatments
- Most iris cysts do not require treatment.
- Treatment is performed for the rare instances of secondary glaucoma or when the visual axis (pupil) becomes blocked. Laser has been used to deflate iris pigment epithelial cysts with minimal side effects.
- The natural history of iris cysts has not been determined. In my experience, some get smaller, some get larger and most stay the same. Until eye care specialists understand which cysts will grow, periodic observation is warranted.