Squamous Carcinoma of the Eyelid
By Paul T. Finger, MD

Description
Squamous carcinomas of the eyelid can locally invade the orbit and sinuses, but rarely metastasizes. It is the second most common malignant eyelid tumor, but is 10 times less common than basal cell carcinoma. This should not be confused with conjunctival squamous carcinoma, which is the most common conjunctival cancer and can spill over onto the eyelid skin.
Symptoms
Squamous eyelid carcinoma can have symptoms that range from the appearance of a hypervascular flat pale, reddish or flaky lesion on the eyelid skin to a thickened well-demarcated reddish, flat tumor surrounded by inflammation (with or without scaling from its surface).
Diagnosis
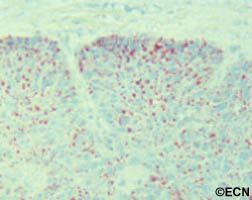
Squamous carcinoma of the eyelid should be photographed at baseline. These lesions can remain unchanged (for years), then invade into the dermis and grow. A simple wedge biopsy can be performed and sent for pathologic evaluation. Once the diagnosis of squamous carcinoma is biopsy proven, definitive treatment is needed.
Treatments
Like basal cell carcinomas, squamous cell cancers of the eyelid rarely metastasize. However, they can grow around the eye into the orbit, sinuses and brain. Therefore, early intervention with complete excision or destruction is warranted.
Surgical approaches depend on the doctors training. Eye care specialists will either perform a planned excision with frozen-section control (of the margins) or the Moh’s Technique. Both types of surgery are used to remove the entire tumor along with a safety zone of normal appearing tissue from the edges of surgical wound (margins). No comparative studies have definitively shown that one technique better than the other. Both surgeries require a cosmetic surgical repair to return eyelid function and cosmesis. When the orbit and sinuses are not involved, local excision is usually curative.
Extension into the orbit and sinuses typically requires more extensive surgery (exenteration, sinusectomy) with subsequent radiation therapy.
At the New York Eye Cancer Center, we have treated select patients with small squamous carcinomas of the eyelid with topical chemotherapy agents or freezing (cryotherapy) using “Finger-tip” applicators. Dr. Finger tries to avoid surgery when possible.