Proton Beam Radiotherapy
By Paul T. Finger, MD
Proton beam radiation therapy is a form of teletherapy, where the radiation is directed into the eye from a machine outside the eye.
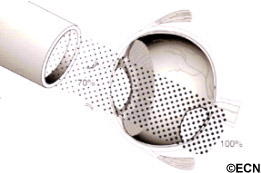
In order to aim the tube-shaped proton beam, surgical clips are sewn (surgically placed) on to the eye, around the tumor’s base. Then the patient returns for 3 to 5 daily outpatient treatments. During treatment, the eye must not move. Eye movement displaces the column of radiation away from the tumor, causing unnecessary radiation of normal ocular structures. Therefore, the eye must be open and closely monitored for movement while the radiation beam is traveling through the eye. If the patient closes their eye, it naturally rotates up “Bell’s Phenomenon” changing the position of both the eye and its tumor.
Eye cancer specialists commonly suggest protons or other external beam treatments when the tumor is touching (juxtapapillary) or surrounding (circumpapillary) the optic nerve. Since beam therapy can include the entire tumor (plus a tumor-free margin), beam therapy is likely to destroy the tumor. However such treatment places the optic nerve within the targeted radiation zone that also results in radiation-related optic nerve damage and loss of vision (in that eye).
Proton beam typically involves directing a column of radiation through the front of the eye (anterior segment, eye lids and/or orbit) in order to reach the intraocular tumor. Since the radiation typically enters the front of the eye, eyelash loss, eyelid excoriation, corneal neovascularization and ulceration, dry eye, neovascular glaucoma, and cataract are more common after treatment with proton beam radiation therapy (compared to low-energy plaque radiation therapy). Some of these effects may occur within weeks of treatment, others may take years to develop.
VS. Eye-Plaque Radiotherapy
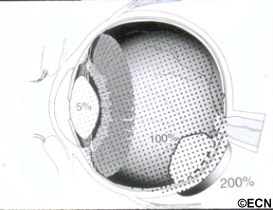
In contrast, Plaque Therapy typically involves attaching a dish-shaped radiation source beneath the tumor and leaving it there for 5-7 days.
Compared with proton-beam, the front of the eye usually receives much less radiation with plaque radiation therapy, but parts of the back of the eye may receive more. This is why anterior “front of the eye” complications (eye lash loss, severe dry eye, neovascular radiation glaucoma) are unusual after low-energy palladium-103 or the older iodine-125 type ophthalmic plaque radiation therapy.
Tumors that touch the optic nerve are more difficult to treat with ophthalmic plaque radiation therapy. Over 12 years ago, Dr. Finger developed specialized “Finger’s slotted plaques” for treatment of tumors the touch or encircle the optic nerve (see below). Due to the advent of super-sized 24 mm (for extra-large tumors) and Finger’s slotted eye plaques (for tumors around the optic nerve), fewer than 6% of patients require enucleation (removal of the eye) as initial treatment for choroidal melanoma (at The New York Eye Cancer Center). Clearly, ophthalmic plaque radiation therapy is the most widely available and most commonly used eye and vision-sparing treatment for choroidal melanoma.
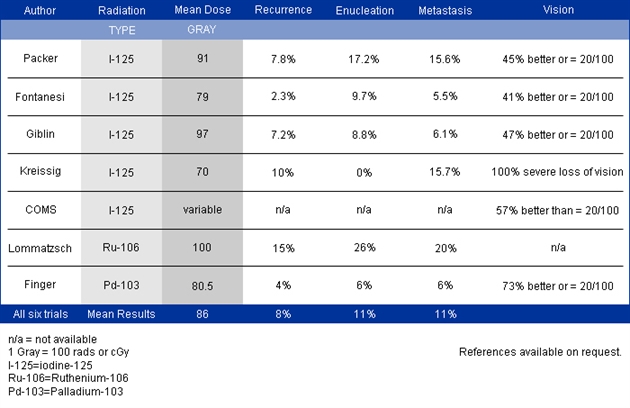
An Overview of Plaque Radiation Therapy in Treatment of Choroidal Melanoma (1,2)
*Note* These results were published largely prior to the discovery of intraocular anti-VEGF therapy for radiation retinopathy and optic neuropathy. To see Dr. Finger’s current results, go to his results page on this web site.
Summary
Currently eye cancer specialty centers should be able to offer radiation as an eye and vision-sparing alternative for 95% patients with intraocular melanoma. The two main types of radiation are eye-plaque brachytherapy (iodine-125, ruthenium-106, palladium-103) and external beam (Proton-Beam, stereotactic radiosurgery). Radioactive plaques are more commonly used and available in more centers throughout the world.
Side effects/complications
An Overview of Plaque Radiation Therapy in Treatment of Choroidal Melanoma (1,2)
Related links
- Scatter laser photocoagulation has been used in an effort to prevent radiation related vision loss.
- Information about the “Finger Classification of Radiation Retinopathy.”
- Compare results using different types of radiation plaques
- About radioactive plaque construction
- Read about Finger’s Slotted Plaques for Tumors Around the Optic Nerve
- Intravitreal Anti-VEGF Therapy For Radiation Retinopathy
References
- Finger PT. Radiation Therapy for Choroidal Melanoma. Survey of Ophthalmology (Review Article) 42:215-32, 1997.
- Finger PT., Berson A, Ng T, Szechter A. Palladium-103 Plaque Radiotherapy for Choroidal Melanoma: An 11-year study. Int. J Radiation Oncology Biol. Phys. Vol 54, No. 5, pp. 1438-1445, 2002.









