Choroidal Melanoma Affecting the Optic Nerve
By Paul T. Finger, MD
Description
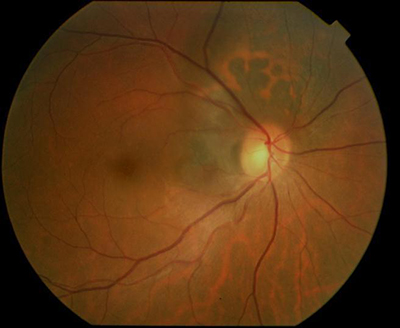 Choroidal melanoma can grow near, touch and even cover the optic nerve. Like other choroidal melanomas, they can exhibit orange pigment on its surface, subretinal fluid (localized retinal detachment), and thickness. The choroidal melanoma in the next photograph exhibits all three findings.
Choroidal melanoma can grow near, touch and even cover the optic nerve. Like other choroidal melanomas, they can exhibit orange pigment on its surface, subretinal fluid (localized retinal detachment), and thickness. The choroidal melanoma in the next photograph exhibits all three findings.
Symptoms
Juxtapapillary choroidal melanoma is typically near the central macular retina and may cause symptoms. Unlike most patients with choroidal melanoma, when the optic nerve is affected patients will have complaints of decreased vision, visual field defects, flashing lights or floaters (spots). However, most choroidal melanomas are found on routine eye examination with dilated ophthalmoscopy.
Diagnosis
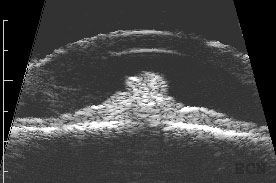
Choroidal melanoma that affects the optic nerve must be differentiated from optic nerve melanocytoma. The eye care specialist will examine the tumor for evidence of orange pigment (lipofuscin, melanolipofuscin), thickness (as measured by ultrasound), for leakage (as measured by photography with angiography), and with optical coherence tomography (OCT).
Unlike optic nerve melanocytoma, malignant choroidal melanoma does not typically spread-out along the nerve fiber layer and are lighter in color. In addition, melanocytoma-OCT findings can be particularly helpful showing tumor cell invasion of the overlying retina and vitreous. In either case, it can be difficult to determine the diagnosis of very small tumors. In these cases, the tumor can be closely watched “followed” for evidence of growth, then a biopsy may need be performed. Dr. Finger has found that melanomas that completely encircle the optic disc (circumpapillary) are likely to cause an afferent pupillary defect.
Treatments
Choroidal melanoma that encircles or covers the optic nerve are particulary difficult to treat with eye-sparing plaque radiation therapy. This is because the optic nerve widens as it leaves the eye into the orbit. In addition, it becomes encased in the optic nerve sheath. Dr. Fingers’ 3D ultrasound studies showed that the nerve nearly triples in diameter behind the eye. Therefore, if a plaque is perfectly placed on the back of the eye, it can only reach to 1.5 mm from the optic disc (effectively missing the rest of the uncovered melanoma. This is why, many patients with melanomas touching or surrounding the optic disc were treated by removal (enucleation) of the affected eye.
Now with 12-years follow up, 94% of patients with choroidal melanoma do not have to lose their eye. For those tough to peripapillary, juxtapapillary and even circumpapillary melaoma, Dr. Finger invented 8-mm slotted plaques. The slot accomodated the entire optic nerve sheath into the plaque, thus allowing the plaque radiation to completely cover and surround the cancer. Fingers’ Slotted Plaques have been able to control more than 98% of these melanomas, has been able to spare some vision (with subsequent intensive anti-VEGF therapy) and allow patients to keep their eye. The patient must be counseled that they are at risk for impaired vision in the irradiated eye.
Related Links
Pearl Cyst of the Iris
By Paul T. Finger, MD
Description
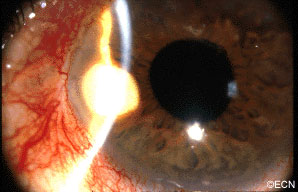
A rare complication of cataract surgery, the “pearl-cyst” may grow from on and within the iris. The tumors are thought to be caused by displaced conjunctival or epidermal epithelium. Rupture of these mucous-containing cysts (within the eye) can cause severe glaucoma.
Symptoms
Most patients present due to ocular inflammation. They may notice the white tumor growing
on the iris.
Diagnosis
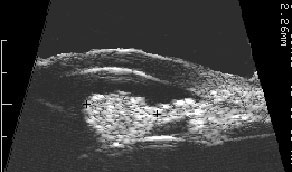
The diagnosis of “Pearl Cyst” should be considered when a patient who has had intraocular surgery (cataract, corneal transplant, or filtering for glaucoma) presents with a slowly
enlarging white iris stromal tumor. High-frequency ultrasound imaging will show three layers: an outer mantle, a low reflective mucus
layer and a central, high-reflective cholesterol crystal core.
Treatments
When “Pearl-cyst” of the iris is suspected, complete surgical excision is warranted. Though difficult, the surgeon should try to remove the cyst intact. Should the cyst rupture during removal, the surgeon should be ready to aspirate or removal the cyst contents. The mucoid contents have been reported to cause secondary glaucoma. If the outer epithelial layer, the mantle, is left behind one runs the risk of cyst recurrence.
Related Links
Iris Melanoma
By Paul T. Finger, MD
Description
The iris is the colored part of the eye. It is made up of two layers. The outer “stroma” can be blue, hazel, green or brown. The back layer (the iris pigment epithelium) is always brown. Tumors can grow within, through and thus behind the iris.
Symptoms
Iris melanoma patients usually have no symptoms. The tumor might be noticed by the patient, their family, or by the eye care specialist (during a routine eye examination). Some people have lots of freckles on their irides. Some of these pigmented spots have thickness and are called Nevi.
If the patient notices that one of their nevi has changed, enlarged or is pulling (ovalization) on the pupil; they should see an eye care specialist for evaluation and referral to an eye cancer specialist.
Diagnosis
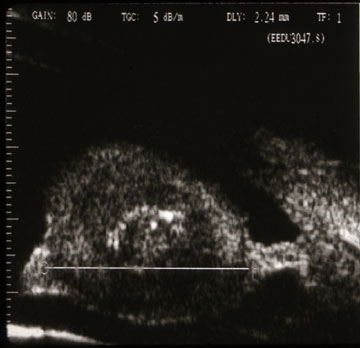
Photographs of the surface of the iris tumor should be obtained to establish a baseline for
future comparisons. High frequency ultrasound is used to examine and measure the iris tumor. Ultrasound can reveal if the tumor is cystic or solid, how it extends within the iris and ciliary body. Ophthalmic oncologists use high frequency ultrasound measurements to evaluate iris tumors for evidence of growth or regression after treatment.
Characteristics that suggest that an iris tumor is cancerous include seeing blood vessels within the tumor (intrinsic vascularity), secondary glaucoma, evidence that the pupil is deformed (ectropion uveae), and the development of a cataract beneath the tumor. Some eyes may have enlarged “sentinel” blood vessels on the white of the eye (sclera) in the quadrant of the tumor.
The most important finding is documented growth. Since iris melanomas are commonly small, and less commonly (10-11%) spread to other parts of the body, these tumors are often watched for evidence of growth or change before biopsy or treatment is considered. A small amount of growth is not thought to significantly affect the rate of metastasis from a small iris melanoma. When necessary, eye cancer specialists can biopsy an iris tumor to help determine if the tumor is benign or malignant.
Treatments
Most pigmented iris tumors do not grow. They are photographed and monitored with periodic observation. When an iris melanoma is documented to grow, we know that it can damage the eye, cause secondary glaucoma and spread to other parts of the body. Then treatment risks become more acceptable to the patient. At The New York Eye Cancer Center, we typically use plaque radiation to destroy iris and iridociliary melanomas. This treatment allows for preservation of the iris, the pupil and does not cloud the cornea. We have found that the most common complication is cataract and permanent vision loss is rare.
Small Iris Melanomas:
Though most small iris melanomas can be surgically removed, however iridectomy may cause glare and astigmatism. The function of the iris and size of the pupil are better preserved if the tumor is destroyed with plaque radiation.
Medium-sized Iris Melanomas:
Though many of these tumors can be surgically removed, plaque or proton radiotherapy should be considered as primary treatment for these tumors. Though a radiation cataract is likely to develop, due to the distance between the radiation and the macular retina, vision limiting radiation retinopathy is very unlikely.
Large-sized Iris Melanomas with Advanced Glaucoma:
These cases can often be difficult to treat with either surgical removal or eye-sparing radiation therapy. Cure for these tumors is likely to require removal of the eye.
Diffuse Iris Melanomas:
Sometimes the entire iris is filled with melanoma. In these cases, removal of the eye is a reasonable option. However, there has been a recent trend towards and our experience that eye and vision-sparing radiation of the entire front of the eye (anterior segment) can be used to control the tumor, spare vision and allow the patient to keep their eye.
Related links
- Read About Radiation for Iris and Ciliary Body Melanoma
- Read the Scientific Literature about Iris Melanoma
- Read About Dr. Finger’s Small Incision Iris Biopsy Technique (or Finger Iridectomy Technique)
- Search PubMed for Iris Melanoma
- Search the Internet about Iris Melanoma
- Read About a Multicenter International Study fo Iris Melanomas
Iris Melanocytoma
By Paul T. Finger, MD
Description
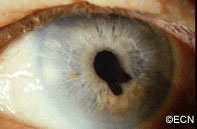
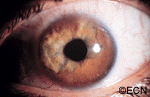
Melanocytoma is a form of nevus that can occur in and behind the iris in the ciliary body. In the image seen below, this melanocytoma has a cobblestone textured surface and feathered margins. Interestingly, it is also causing a small amount of pupillary distortion (correctopia). Bits of iris melanocytoma can break off and settle in the inferior angle. These sedimentary melanocytoma cells can clog the natural drain of the eye (trabecular meshwork), causing increased eye pressure (glaucoma). Melanocytoma tumors can grow, malignant transformation is rare and metastasis is reportable.
Symptoms
Most patients with iris melanocytoma can see a dark spot on their iris, and have no other symptoms. Patients can have pigment dispersion, secondary glaucoma and intraocular inflammation (iritis). Secondary glaucoma can either be asymptomatic, cause one-sided (ipsilateral) headaches and cloudy vision (with halos around lights).
Diagnosis
Iris melanocytoma can be diagnosed by clinical examination. The tumor tends to be dark brown to black and the edges feather-shaped. The surface can be cobblestone (bumpy) appearance or smooth.
High-frequency ultrasound is particularly helpful for the diagnosis of iris melanocytoma. This technique is used to evaluate the depth of penetration into the iris and surrounding tissues. It can also be used to monitor for growth. These tumors can extend through the iris and into the ciliary body. Unlike low reflective iris melanomas, they tend to appear bright (highly reflective).
Treatments
Iris melanocytoma does not usually require treatment. High-quality slit-lamp and gonioscopic photographs should be taken to record the appearance and surface characteristics of the tumor. High-frequency ultrasound should be performed to evaluate its thickness and extension into surrounding structures. These evaluations will be used to monitor for growth. Careful attention should be made to measuring intraocular pressure. Secondary glaucoma can occur due to pigment that clogs the natural drain of the eye (trabecular meshwork). Patients should keep a copy of these baseline tests in case they move to another area or their doctors change.
Should an iris melanocytoma be found to grow, an iris biopsy can be performed to determine if it is benign or malignant. When possible, rapidly growing and malignant iris melanocytomas whould be surgically removed. If resection is not possible, they can be treated with relatively high-dose plaque radiation therapy.
Additional info
Secondary melanocytomalytic glaucoma can be treated like other glaucomas. It is reasonable to consult with a glaucoma specialist. Strenuous exercise may “shake-up” the intraocular pigment and cause a temporarily increased eye pressure. When this happens, patients may notice headaches or cloudy vision after exercise.
If glaucoma surgery is recommended (e.g. trabeculectomy, stent, valve), a tumor biopsy can ensure that the tumor is not a melanoma.
(See Innovations Section – Finger Iridectomy Technique).









