Chronic Lymphocytic Leukemia
By Paul T. Finger, MD
Description
Leukemia is a systemic disease that can involve the eyes. It occurs in both children and adults. In that the eyes can be a relative sanctuary (a place to hide from systemic chemotherapy) for leukemic cells, intraocular recurrences have been reported after both total body irradiation and systemic chemotherapy. It is reasonable for all patients with leukemia to have periodic eye examinations.
Adults can also have leukemia and develop infiltration of the eyes. The case presented in this section (below) demonstrates one such case.
Symptoms
Depending on the location of the leukemic infiltrates, patients will have different symptoms. Most patients are found to have retinal tumors with hemorrhage, optic nerve swelling (papilledema) or cells in the anterior chamber of the eye (hypopyon/hyphema). Leukemic tumor called “chloroma” can also form around the eyes and in the orbit.
In this case, posterior uveal infiltration caused thickening of the choroid that moved the retina forward. This made the patient more far-sighted (hyperopic shift) due to a shortening of the distance between the cornea/lens complex and the retina.
The front of the eye was also infiltrated by leukemic cells. Thickening of the iris, ciliary body and anterior uvea induced a secondary “narrow angle” glaucoma. The symptoms of glaucoma include seeing haloes around lights, headache (brow-ache) and eye pain.
Diagnosis
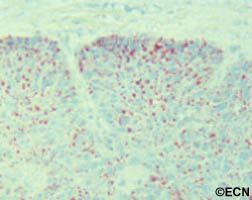
The clinical diagnosis of infiltrative ocular leukemia (e.g. typical findings and a history of systemic leukemia) is typically adequate for treatment of patients. When proof of recurrence is needed to proceed with systemic or local therapy, a biopsy may be performed for a cytologic or histopathologic diagnosis.
Treatments
The treatment of intraocular leukemia is (in part) dependent on the treatment of the patient’s systemic disease. For example, in the clinical situation where the eye findings are not posing an immediate threat to vision, your physician my wait for systemic therapies to resolve the ocular disease. In cases where all standard treatments have been unsuccessful in resolving the ocular leukemia; patients will be treated with low-dose external beam radiation therapy.