Research Breakthrough: Using Immunotherapy to Fight Uveal Melanoma
A new study suggests patients diagnosed with uveal melanoma could benefit from immunotherapies that harness the body’s own anti-tumor T-cell populations.

Uveal melanoma is a cancer of the eye involving the iris, the muscle surrounding the lens, or the choroid – a vascular layer with connective tissue between the retina and the sclera. It is a rare form of eye cancer with no effective therapies once it spreads to other parts of the body.
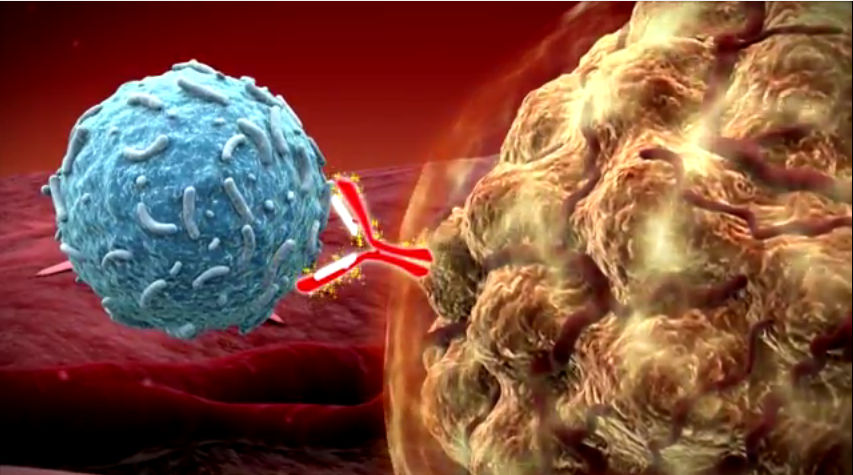
Uveal melanoma is related to more common cutaneous (skin) melanoma. Doctors have had success treating skin cancers with immunotherapies that boost naturally existing anti-tumor T-cell responses. In essence, this approach boosts the body’s natural immune system response to fight the tumor.
For instance, a drug called Keytruda was used to successfully treat Jimmy Carter’s melanoma. But despite the success of immunotherapy in attacking more common skin cancer tumors after it spreads, the role of this type of treatment for metastatic uveal melanoma remains unclear.
Fifteen researchers from the National Cancer Institute and other institutions embarked on a study to determine if this type of anti-tumor immune response exists against uveal melanoma.
To conduct the study, researchers surgically procured metastases from the livers of eye cancer and skin cancer patients. They then compared the tumor cell structures along with their associated T-cells using a variety of techniques.
Researchers found that despite the fact both are related to melanoma, the tumor cells differed in melanin content, the antigens provoking an immune response, and in their genetic mutations. The T-cells attacking the tumors were also different. Researchers found that anti-tumor T-cells in cutaneous melanoma were predominantly CD8+ while those in uveal melanoma were CD4+ dominant.
While the effectiveness of T-cells against the tumors was much higher in cutaneous melanoma, researchers found a subset of T-cells in uveal melanoma that had robust anti-tumor reactivity, comparable in magnitude.
Researchers say the absence of melanin pigmentation in the original tumor, before it metastasized to the liver, strongly correlated with the production of highly effective T-cells. In other words, a group of uveal melanoma tumors with lower melanin levels do seem to produce a promising immune system response that attacks the tumor
Knowing that a subset of uveal melanoma tumors with the ability to provoke an immune response exists opens the door to further research. Doctors can build on this knowledge to potentially discover therapies that will boost anti-tumor T-cell production and/or effectiveness to successfully treat this form of eye cancer even after it spreads..