Right alongside cancers of the breast and lung, skin cancer exists as a well-known cancer afflicting U.S. Americans. The history of cancer study has lead to the identification of over 200 types of the disease, and skin cancer is the most commonly diagnosed of them, affecting more than 1 million Americans a year. Information on this type of cancer has been widely disseminated to the American public, from a fleet of dedicated websites, to news articles, and more, to the extent that most American adults realize that skin cancer can often arise from dangerous exposure to ultraviolet (UV) sunlight. But did you know that skin cancer and eye cancer, a lesser-known type of cancer, are closely linked? Indeed, skin cancer can negatively affect the eyes — take seventy-year-old John McPartland for example, who understood this well.
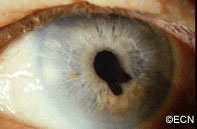
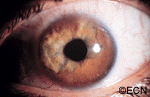
In 2001, McPartland, a lifetime lover of outdoor activity, noticed a freckle on his eyelid. Determined to find answers, he consulted with many doctors until finally meeting with Dr. Paul T. Finger, who diagnosed McPartland with conjunctival melanoma. A melanoma is a particular type of skin cancer; it affects nearly 70,000 people, and is found on the melanocyte cells of the skin. Melanocyte cells are responsible for the production of brown skin pigment — melanin, Because these pigment-producing cells are afflicted, melanomas commonly begin as pigmented, odd-looking freckles like McPartland’s. The conjunctiva is a delicate, clear membrane covering the inside of the eyelids and the white (sclera) of the eye. McPartland’s diagnosis was deadly.
“I just thought I should check it out and see if it is anything,” McPartland said, “and fortunately I did … As far as I’m concerned, [Dr. Finger] saved my life.”
About 2,400 patients are diagnosed with conjunctival melanoma every year, often in part due to the same UV light that causes skin damage. Those who work outdoors, play sports and/or frequent beaches are most vulnerable to eye cancer. Having light blue eyes and a fair complexion increases vulnerability, due to a lack of melanin (brown pigment) production that protects us from harmful sun exposure. Those who have a family or personal history of skin cancer are also vulnerable. For these people, Dr. Finger recommends that they “should have an eye exam, and then every six months thereafter.”
“Certain drugs also increase UV toxicity” Dr. Finger additionally cautions. “Patients who take chlorothiazides, sulfonamides, tetracycline, phenothiazins, psoralens, and allopurinol should be extra cautious about sunlight.”
A 2008 Fox News article highlights Dr. Finger’s experience with McPartland, along with his advice for optimizing eye health that he continues to recommend to his patients today. While the importance of wearing hats and using sunblock to protect the skin has long been stressed to the American public, Dr. Finger says people should approach this thinking to the eyes as well. The best way one can optimize eye health on their own? Using UV-blocking sunglasses!
“Think of sunglasses as sunblock for your eyes”, Dr. Finger says. He advises that sunglasses with 100% UV protection offer optimal prevention of sun damage to the eye.

Cancer is certainly a difficult reality to endure for many people, but there are ways one can help to protect themselves against the disease. By doing something as simple as wearing UV-blocking sunglass, you can take charge of your health today.
Stay tuned for more stories at eyecancer.com by keeping our website in your bookmarks!