NYECC’s How-To for Chemotherapy Eye Drops
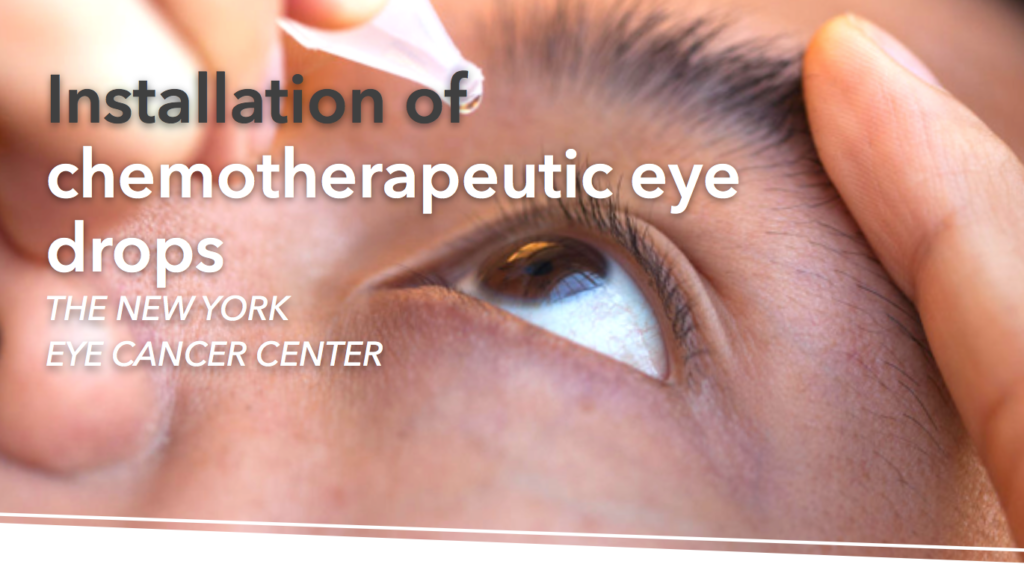
Whether treating a dry eye through artificial tears or over-the-counter anti-allergy drops, many people around the word have experienced using eye drops in their every day drops — however, using chemotherapy drops to treat malignant eye tumors may seem daunting. You may be wondering how these eye drops differ from simple artificial tears, what specific instructions, or additional precautions must be made to install them into the eye, and so on. Luckily, the New York Eye Cancer Center has written a comprehensible step-by-step process that can help put your mind at ease when understanding chemotherapy drops.
Before you read the instructions, here are some helpful reminders and tips regarding your drops:
Put one drop in the affect eye 4 times a day, while awake, for the directed amount of time. You may administer the drops to your own affected eye by yourself, or you may have someone else do it for you. Remember to refrigerate your drops at all times! If you plan on being outside for the majority of your day, keep your drops in an insulated bag with ice packs. Do not put your drops in the freezer.
Now, regardless of the drops you are using (for example, interferon A or 5-FU), please take care to follow these instructions.
STEP 1: Sterilization is important — wash your hands! If possible, put on latex gloves.
STEP 2: Lie down flat, or recline in a chair.
STEP 3: Look down, pulling back your upper eyelid.
STEP 4: Put the drop on the top part of your eye.
STEP 5: Slowly close your eye, keeping it closed for 5 minutes.
STEP 6: If there is any excess, gently wipe it away.
STEP 7: Sterilization remains important! If you did not put on gloves, wash your hands again.
And of course, should you be experiencing any eye pain, blurred vision, or flu-like symptoms, do not hesitate to contact NYECC at 212-832-8170.
Want to keep this information on hand at all times? We have put this information into a simple PDF available for download. You can download and print this PDF to keep with you by clicking here.

 From the summer of 2016 to 2017, Dr. Sonal Chaugule gained a wealth of knowledge as an Eye Cancer Foundation (ECF) fellow under the tutelage of Dr. Paul T. Finger at the NYECC. From shadowing Dr. Finger’s surgeries at the New York Eye and Ear Infirmary, to speaking at the Second Eye Cancer Working Day in March 2017, Dr. Chaugule has since returned to India, using the knowledge she has gained as tools to continue in the footsteps of her mentors. Her efforts manifest in
From the summer of 2016 to 2017, Dr. Sonal Chaugule gained a wealth of knowledge as an Eye Cancer Foundation (ECF) fellow under the tutelage of Dr. Paul T. Finger at the NYECC. From shadowing Dr. Finger’s surgeries at the New York Eye and Ear Infirmary, to speaking at the Second Eye Cancer Working Day in March 2017, Dr. Chaugule has since returned to India, using the knowledge she has gained as tools to continue in the footsteps of her mentors. Her efforts manifest in