Last fall, The Eye Cancer Foundation hosted a retinoblastoma workshop in Guangzhou, China.
The primary goal was to deliver systematic training in retinoblastoma management based on the general principles of the origin and development of the disease. But the workshop went beyond practical training. It served to build strong relationships among all of the participants.

Eleven faculty members interacted enthusiastically with 19 students. The students included practicing ophthalmologists, oncologists, pathologists, and radiologists. These medical professionals already cared for retinoblastoma patients in their daily work, but they generally lacked the opportunity to discuss the science and rationale behind the treatment with others.
You can watch videos of the workshop sessions here.
The extensive effort the faculty put into their presentations was evident in the discussions, which included topics ranging from core treatment modalities, to fundamental molecular mechanisms in retinoblastoma, to social and life issues facing patients’ families. Eager students engaged in active dialogue, which even extended into breaks. The students left the workshop possessing greater depth of knowledge and new ideas for treating retinoblastoma in China.
The workshop also kicked off a long-term project. Students left with homework: all of the students filled out a table outlining their opinions of care options for a child presenting with IIRC1 Group D eye. This homework is first step in a study of informed consent for retinoblastoma families, and all participants of the workshop will be co-authors.
The Eye Cancer Foundation has a video library of the workshop talks that will be posted on the organization’s website to benefit students worldwide.
The long-term impact of the workshop is still being measured. All participating students filled out pre-workshop and post-workshop assessments to gage their knowledge of retinoblastoma. Once the videos are available in China, and students have an opportunity to review them, we will conduct additional questionnaires.
Comments from the students reveal just how valuable the workshop was.
“..these lectures in Guangzhou touched me deeply.”
“…such a wonderful workshop…very comprehensive training of retinoblastoma, covered overall content of RB from epidemiology, genetic, pathology to clinical treatment. The excellent talks and heated discussion refreshed my knowledge and will help me to improve my clinical treatment of RB.”
“So glad to have this opportunity…We learned much more updated knowledge about RB.”
“I benefited a lot from this training”
“Deeply indebted …for the comprehensive lessons in RB Workshop”
“After the training, I have a deep understanding about retinoblastoma.”
“The most important thing I learn is cooperate. We can’t fight the disease alone.”
“I learned much in this meeting and workshop. Lack of experience in diagnosis and treatment, I did not exchange with experts, but I have the chance to consult some domestic counterparts.”
ick here to watch the workshop videos.
1. Murphree AL. Intraocular retinoblastoma: the case for a new group classification. Ophthalmology clinics of North America. 2005;18:41-53.
2. Mallipatna AC, Gallie BL, Chevez-Barrios P, Lumbroso-Le Rouic L, Chantada GL, Doz F, Brisse HJ, Munier FL, Albert DM, Catala-Mora J, Desjardins L, Suzuki S, Carroll WL, Coupland SE, Finger PT. Chapter 68: Retinoblastoma Ophthalmic Sites: Part XV The AJCC Cancer Staging Manual, 8th edition. Editor in Chief, Mahul B. Amin, Ed. Board: Edge, SB, Byrd, DR, Compton, CC, Fritz, AG, Greene, FL, Trotti A. New York, Springer 2017, pp. 819-831.
The Eye Cancer Foundation Retinoblastoma Workshop
GuangZhou, China November 28- 30, 2016
Purpose
- Systematic retinoblastoma management training
- Understand general principles of pathogenesis of retinoblastoma
Duration: 3.5 days
Trainees: 12-15 doctors
Trainers:
Dr. Junyang Zhao, Beijing Children’s Hospital, China;
Dr. Xiaoli Ma, Pediatric Oncology, Beijing Children’s Hospital, China
Dr. Bin Li, Beijing Tongren Hospital, China
Dr. Jing Zhang, Guangzhou Women and Children Medical Center, China
Dr. Brenda Gallie, Director Retinoblastoma Program, SickKids Hospital, Professor University of Toronto, Canada;
Dr. Tero Kivelä, Helsinki University Central Hospital, University of Helsinki, Faculty of Medicine, Helsinki, Finland;
Professor David Mackey, Perth, Australia;
Professor Sandra E. Staffieri, Centre for Eye Research Australia
Dr. Francis Munier, Head, Ocular-oncology Unit, Jules Gonin Eye Hospital, Professor, Faculté de biologie et de medicine de l’UNIL, Lausanne, Switzerland;
Dr. Bhavna Chawla, Ocular Oncology Service, Rajendra Prasad Centre for Ophthalmic Sciences, All India Institute of Medical Sciences, New Delhi, India;
Dr. Vikas Khetan, Ocular Oncology Service, Senkara Nethralaya, Chennai, India;
Dr. Wantanee Dangboon, Department of Ophthalmology, Faculty of Medicine, Prince of Songkla University, Hat Yai, Songkhla, Thailand;
Dr. Pamela Astudillo, Medical Specialist III, Jose B Lingad Memorial Regional Hospital, Consultant, Angeles University Foundation Medical Center, The Philippines;
Ms. Sandra E. Staffieri, PhD Candidate, Clinical and Research Orthoptist,Centre for Eye Research and Retinoblastoma Care Co-ordinator, Department of Ophthalmology, The Royal Children’s Hospital, Melbourne, Australia.
Schedule
Day 1: Monday, November 28, 2016:
8:20-9:50 Geographic and world perspective
Dr. Junyang Zhao, Dr. Brenda Gallie, Dr. Tero Kivelä
- (10 min) Workshop strategy and Questionnaires #1/3
- (30 min) History of global retinoblastoma treatments: enucleation, radiotherapy, chemotherapy, focal chemotherapy modalities, etc. (Brenda Gallie)
- (30 min) World epidemiological trends of retinoblastoma, especially in Asia-Pacific. (Tero Kivelä)
- (20 min) History of retinoblastoma in China (Junyang Zhao)
9:50-10:10 Tea Break
10:10-11:40 2016 collaborative care and innovations
Drs. Junyang Zhao, Brenda Gallie
- (20 min) Chinese retinoblastoma collaboration. (Junyang Zhao)
- (30 min) 1RBW map & meeting, classification/staging. (Brenda Gallie)
- (40 min) eCancerCareretinoblastoma (eCCrb) for patient care and research. (Brenda Gallie)
11:40-13:20 Lunch
13:20-14:50 Systemic chemotherapy
Drs. Xiaoli Ma, Dr. Bhavna Chawla
- (30 min) Systemic chemotherapy and management. (Xiaoli Ma)
- Mechanism of drugs, dosage, side effects.
- (20 min) Multi-modal therapy for extra-ocular retinoblastoma. (Xiaoli Ma)
- High-dose chemotherapy and stem cell rescue
- Adjuvant chemo for high risk pathology
- (20 min) Systemic chemotherapy for intra-ocular retinoblastoma. (Bhavna Chawla)
- (20 min) Neo-adjuvant chemo for extra-ocular retinoblastoma. (Bhavna Chawla)
14:50-15:10 Tea Break
15:10-16:40 Genetic testing and counseling
Drs. David Mackie, Sandra E. Staffieri, Wantanee Dangboon,
- (30 min) Principles of genetic knowledge and counseling. (David Mackey)
- (20 min) Genomic forefront for the future. (David Mackey)
- (20 min) Low vs full penetrance RB1 mutations and mosicism (Brenda Gallie)
- (20 min) Genetic testing for retinoblastoma – the changing paradigm for clinical care. (Sandra Staffieri)
- (20 min) Life-long surveillance for retinoblastoma and second cancers. (Wantanee Dangboon)
16:40-17:00 Tea Break
17:00-17:40 Day review and free discussion
Day 2: Tuesday, November 29, 2016:
8:20-9:50 Pathology
Drs. Xialin Xi, Brenda Gallie
- (30 min) Pathogenesis of retinoblastoma. (Brenda Gallie)
- (30 min) pTNM and pathology report. (Brenda Gallie)
- (15 min) Critical observations, communication, actions. (Xialin Xi)
- (15 min) High-risk eye pathology features & indication for adjuvant chemotherapy. (Brenda Gallie)
9:50-10:10 Tea Break
10:10-11:40 Examination staging and screening
Drs. Vikas Khetan, Tero Kivelä
- (30 min) Presentation and diagnosis. (Vikas Khetan)
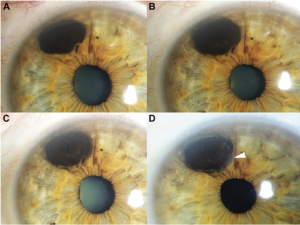
- (30 min) 2017 TNMH vs 2005 IIRC (Vikas Khetan)
- (15 min) Neonatal retinoblastoma. (Tero Kivelä)
- (15 min) Trilateral retinoblastoma. (Tero Kivelä)
11:40-13:20 Lunch
13:20-14:50 Focal therapies
Drs. Francis Munier, Jing Zhang, Jungyang Zhao, Pamela Astudillo
- (15 min) Intravitreal and Intra-arterial chemotherapy for retinoblastoma. (Francis Munier)
- (15 min) Laser/cryo, plaque. (Francis Munier)
- (20 min) Technique, dos and don’ts of selective intra-artery chemo. (Jing Zhang, presented by Drummond Xia)
- (20 min) Enucleation, Myoconjunctival technique, Prosthetic conformers and eyes. (Pamela Astudillo)
- (20 min) Intraocular tumor resection. (Junyang Zhao)
14:50-15:10 Tea Break
15:10-16:40 Clinic and Basic Research Opportunities
Dr. Tero Kivelä
- (30 min) World surveys and analysis of outcomes (Tero Kivelä)
- (30 min) Standardization of care (Tero Kivelä)
- (30 min) Basic statistical principles for clinical reports (Tero Kivelä)
- (15 min) Role of eCCRB (Brenda Gallie)
16:40-17:00 Tea Break
17:00-17:40 Day review and free discussion
Day 3: Wednesday, November 30, 2016:
8:20-9:50 Collaboration
Drs. Junyang Zhao, Jing Zhang, Xiaolin Xia, Francis Munier, Tero Kivelä, Brenda Gallie, Vikas Khetan, Bhavna Chawla, David Mackie
- National China
- National India
- EuRBG
- 1RBW
9:50-10:10 Tea Break
10:10-10:30 Genetic consultant and explanation of Impact/Geenseq reports. (Marc Zhao)
10:30-11:30 Knowledge Summary and Review
All participants
12:00 Check-out
Six months after the Workshop, we request all participants to fill out Questionnaire #3/3, on line.
 Castle Connolly’s top doctors are nominated by their peers through an extensive survey process of thousands of American physicians. Each year, Castle Connolly receives nearly 100,000 nominations through this process. The organization’s research team screens medical education, training, board certifications, hospital appointments, disciplinary histories, and other information to determine the best doctors in America.
Castle Connolly’s top doctors are nominated by their peers through an extensive survey process of thousands of American physicians. Each year, Castle Connolly receives nearly 100,000 nominations through this process. The organization’s research team screens medical education, training, board certifications, hospital appointments, disciplinary histories, and other information to determine the best doctors in America.