Glossary
A
Adnexa
[Add-Nex-ah]
Appendages. Structures around the eye that support and surround it (e.g. the eye lids).
Alopecia
[Ah-lo-pee-Sh-ah]
Loss of body hair.
Alternative Treatment
Treatment other than the standard or most common treatment of a condition.
Anesthesia
[Ann-es-Thee-zee-ah]
Absence of normal sensation, usually a drug-induced decreased sensitivity to pain.
Apoptosis
[A-pop-Toh-sis]
A form of cell death where a programmed sequence of events leads to the elimination of cells without releasing harmful substances into the surrounding area.
B
Benefit
[Ben-eh-Fit]
The possibility of improvement (e.g., saving sight and saving life) by use of a diagnostic method or treatment.
Benign
[bee-NI-en]
The tendency to stay the same and not spread to other parts of the body.
Bias
[Bye-ass]
Personal preference not based on facts.
Biopsy
[Bye-op-see]
The removal of tissue, cells or fluids from the body for examination or study.
Brachytherapy
[Bray-key-THER-uh-pee]
Implanted radiation. For example, radiation treatment delivered by a small plaque sewn to the outside of the eye (sclera).
C
Cancer
[Can-sir]
A general term for more than 100 diseases characterized by an abnormal uncontrolled growth of cells. Cancerous tumors can invade and destroy surrounding normal tissues and/or spread to other parts of the body.
CAT Scan (aka computed axial tomography)
[KAT SKann]
An x-ray technique that uses computerized reconstruction to form an image of the inside of the body (head, orbit, chest, abdomen).
Chemotherapy
[KEY-mo-THER-uh-pee]
The use of topical or systemic drugs to treat cancer.
Choroid
[KO-royd]
Layer of normal blood vessels [vascular-layer] of the wall of the eye. The choroid is located between the retina and the sclera.
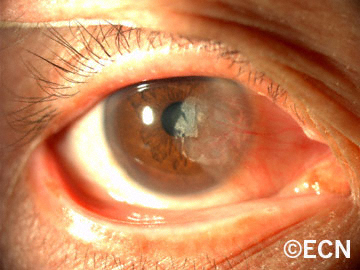
Choroidal Melanoma
[Ko-ROY-dull Mel-uh-NO-muh]
A malignant tumor (cancer) of the vascular “choroidal” layer of the eye, made up of pigment producing cells (melanocytes).
Chromosome 13
[Kro-moh-Some 13]
The piece of DNA that is responsible for the development of retinoblastoma.
Ciliary Body
[Silly-Airy Body]
An organ located right behind and encircling the iris. Tumors can come from the vascular and non-vascular parts of the ciliary body. The ciliary body also makes fluid which fills the eye.
Clinical Trial
[Klin-ick-al Try-ul]
The systematic investigation of the effects of specific treatments according to a formal research plan.
Complication
[Kom-plick-A-shun]
Undesirable effect of a disease or its treatment that can change the outcome and may require additional treatment.
COMS
Collaborative Ocular Melanoma Study. The largest prospective randomized clinical trial conducted to investigate choroidal melanoma.
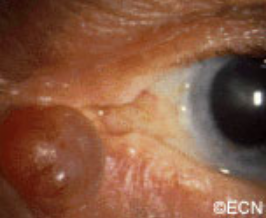
Conjunctiva
[Con-junk-Tie-Vah]
A thin membrane that covers most of the outside of the eyeball and inside the eyelids.
Conjunctivitis
[Con-junk-Ti-Vie-tiss]
Inflammation or infection of the thin membrane that covers most of the outside of the eyeball and inside the eyelids.
Cornea
[KOR-nee-uh]
The clear outer portion of the eye which covers the iris and admits light through the pupil.
Cryotherapy
[KRY-oh-THER-uh-pee]
The destruction of tissue or tumor by the application of extreme cold.
Cyclotron
[SY-klo-tron]
A machine which creates high-energy radiation beams.
D
Depth Perception
The ability to recognize 3-dimensional objects and their relative positions in space.
Diagnosis
[dye-egg-NO-sis]
The name of a disease or condition.
Dormant
[DOR-mant]
A relatively inactive or resting condition in which some processes are slowed down or suspended.
Dosimetry
[Doe-si-met-tree]
The act of calculating the amount of treatment (e.g. radiation).
E
Enucleation
[e-noo-klee-AY-shun]
Removal of the eyeball, leaving the eye-muscles and other contents of the eye socket.
Equator
[EE-KWAY-Tore]
A circular position that divides the front from the back portion of the eye.
Eye Wall Resection
[eye-wall ree-SECK-shun]
Removal of the portion of the eye that contains the tumor.
F
Fluorescein Angiography
[FLOR-uh-seen an-jee-OG-ruh-fee]
A test where a vegetable dye is injected into a vein, allowed to circulate within the eye while photographs of the intraocular circulation are recorded.
Fovea
[Foe-Vee-ah]
The center of the macular retina primarily responsible for both color vision and fine resolution (reading vision).
G
General Anesthesia
[JEN-er-ruhl ann-es-THEE-zee-ah]
A complete drug-induced absence of sensation and consciousness induced by an anesthesiologist during surgery.
H
Hemangioma
[Hee-Man-gee-Oh-Ma]
Congental or acquired tumor comprised of blood vessels.
Hemorrhage
[HEM-or-ridge]
Loss of blood, either inside or outside the body.
I
Implant
[Im-Plant]
A device which is placed inside. For example, an implant is placed into the orbit to make up for the loss of the eyeball during enucleation surgery.
Informed Consent
[In-formd Kon-sent]
The process where a patient learns about all the aspects of a medical treatment or clinical trial before agreeing to participate. This process should include a detailed explanation of the potential risks and benefits of all standard medical procedures and treatments.
Interferon
[In-ter-Fear-on]
A immune system modulator used to treat conjunctival and corneal cancers. This chemotherapy drug is either used as an eye drop and/or injected around the tumor.
Iodine-125 Seeds
[I-O-dine 125 seeds]
Rice-sized radioactive sources which are typically purchased and glued within gold eye-plaques for use in treatment of intraocular tumors.
IRB
[Institutional Review Board]
A committee of people who typically reviews, approves or denies the right to conduct a scientific study. IRB’s assure that such studies are ethically and scientifically proper.
Irradiate
[ear-Ray-dee-ate]
To expose part of the body to diagnostic or therapeutic radiation.
J
Juxtafoveal
[Jux-Tah-Foe-Ve-al]
Located next to (touching) the fovea.
Juxtapapillary
[Jux-Tah-pap-hill-airy]
Located next to (touching) the optic nerve.
K
Keratitis
[Ker-ah-tie-tis]
Irritation or inflammation of the cornea. Keratitis can be due to exposure, radiation, infection, or immune reaction.
L
Laser
[LAY-zur]
A very narrow, high intensity, light, which can burn tissue and/or join structures together.
Lens
[Lenz]
A clear structure behind the pupil, which helps to focus light onto the retina.
Local Anesthesia
[LOW-cull ann-es-THEE-zee-ah]
The patient is awake but drugs have been given to decrease or stop sensation in the area of surgery.
Lymphangiectasia
[limf-an-gee-eck-tae-Z-ah]
A dilated lymphatic channel, commonly filled with blood.
M
Macula
[Mack-U-Lah]
The part of the retina responsible for the center of vision.
Malignant
[ma-LIG-nant]
When a tumor contains cancer cells that can spread and cause death.
Melanoma
[mel-uh-NO-muh]
A tumor made up of pigment cells called melanocytes.
Metastasis
[meh-TASS-tah-sis]
The site where the cancer cells have spread to form a tumor.
Metastasize
[me-TAS-tah-size]
The spread of cancer cells from the original tumor to a distant site.
Mitomycin
[My-toe-My-cin]
A chemotherapy drug sometimes used to treat conjunctival and corneal cancers.
Mitosis [Mitotic]
[My-Toe-Sis]
The process when the cell (and its chromosomes) divides.
N
Neovascularization
[Nee-Oh-Vas-Q-lar-eye-zay-shun]
The growth of new blood vessels into, around or within tissue.
O
Ocular
[ock-yu-lar]
Of or pertaining to the eye.
Ocularist
[ock-u-lah-rist]
A specialist who makes and fits artificial eyes.
OD [oculus dexter]
Latin for “right eye.”
Oncologist
[ON-kol-oh-gist]
A general medical doctor who specializes in cancer treatment.
Ophthalmic Oncologist
[off-thal-mick ON-kol-oh-gist]
An ophthalmologist with special training in the diagnosis and management of patients with eye cancer.
Ophthalmologist
[off-thal-mol-loh-gist]
A physician with special training in the medical and surgical treatment of eye diseases.
Optical Coherence Tomography (OCT)
[Op-tic-al Coh-hear-ents Toe-Mah-Graph-E]
Where a laser imaging device is used to image the eye. It can be used to image the front of the eye, but for eye cancers it is most commonly used to observe the retina, choroid and sclera.
Optic Nerve
[OP-tick nurv]
The nerve that sends vision-messages between the brain and the eye.
Optic Neuropathy
[OP-tick nur-Op-ath-he]
Used to describe when the optic nerve appears or functions abnormally.
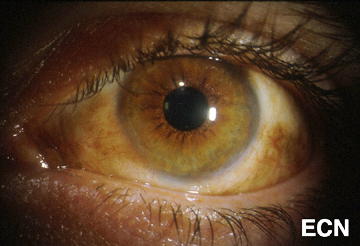
Orange Pigment
Collections of lipofuscin pigment typically seen on the surface of choroidal melanomas or suspicous choroidal nevi.
Orbital Tumor
[oar-bit-tall TOO-mur]
A benign or malignant tumor behind or around the eye.
OS [oculus sinister]
Latin for “left eye.”
OU [oculus uterque]
Both eyes.
P
Palladium-103 Seeds
[pah-lay-dee-um 103 seeds]
Rice-sized radioactive sources which are typically purchased and glued within gold eye-plaques for use in treatment of intraocular tumors.
PET / CT
[Pah-Zit-tron EE-miss-shun Toe-mog-graph-Fee / Cat-skah-hun]
An imaging study that can provide images of the whole body looking for evidence of cancer.
Photocoagulation
[Foe-Toe-Koe-ah-gu-LAY-shun]
The use of intense light (usually laser-beams) to destroy eye tissues, abnormal blood vessels, and/or tumors.
Pigmentation
[PIG-men-tay-shun]
The color of the body.
Pigmented Cells
[PIG-men-ted sells]
Cells, which are colored and usually contain the natural pigment of the skin or eye, called melanin.
Plaque
[plak]
A bowl-shaped device, which is, or can be made radioactive by adding seeds. An ophthalmic plaque is typically sewn to the wall of the eye in order to treat an underlying intraocular tumor. Plaque therapy is the most common treatment for choroidal melanoma.
Primary Cancer
[PRY-may-ree Kan-ser]
The original malignant tumor from which cells can spread to other parts of the body.
Prognosis
[Prog-NO-sis]
What is most likely to happen over time.
Proptosis
[Prop-Toe-Sis]
When the eye is (displaced) pushed forward from its normal position.
Prosthesis
[pross-thee-sis]
A device that is used to replace the appearance and/or function of a removed organ. For example, the plastic eye that is placed beneath the eyelids to simulate a removed eye.
Proton Beam Radiation
[prote-on beem ray-dee-ay-shun]
Radiation made up of protons, which come out of a machine, travel through the eye into the tumor.
Pupil
[pyoo-pill]
The round opening in the iris which lets light into the eye and onto the retina.
R
Radiation
[ray-dee-Ay-shun]
Energy waves which can be used to diagnose (e.g. chest x-rays) or treat diseases (e.g cancers).
Radiation Oncologist
[ray-dee-AY-shun ON-kol-OH-jist]
A physician with special training in the use of radiation to treat diseases.
Radiation Retinopathy
[ray-dee-Ay-shun RET-in-opp-ah-thee]
When large amounts of radiation cause vascular changes in the normal retina often resulting in decreased vision.
Radiation Therapy
[ray-dee-AY-shun THER-ah-pee]
The use of high-energy radiation to treat cancer and certain benign diseases.
Radioactive Plaque
[ray-dee-OH-ack-tiv plak]
A bowl-shaped radiation device which can be used to treat eye cancers (e.g. melanomas and retinoblastomas).
Randomization
[RAN-dum-eye-ZAY-shun]
The process of assigning patients to two or more treatment options, where each patient has an equal chance of receiving each treatment.
Retina
[REH-tin-uh]
The nerve tissue which lines the inside of the eye and acts like the film inside a camera.
Retinoblastoma
[Ret-in-OH-blast-OH-mah]
A cancerous tumor of the retina which typically affects children under 5 years of age. Retinoblastoma is the most common malignancy to start within the eye of children.
Risks
The possibility of loss or injury resulting from a condition or treatment.
S
Sclera
[SKLEHR-uh]
The white outer wall of the eye.
Scotoma
[SkoH-Toe-Mah]
A blind-spot or defect in the field of vision.
Side Effect
An unwanted effect of treatment.
Standard Treatment
The accepted, recognized and commonly used form of therapy. What is typically used by most physicians treating a particular disease.
Stereopsis
[Stay-re-op-sis]
The ability to see objects with depth perception from both eyes.
T
Teratogenic
[Tear-at-Oh-gen-ick]
The tendency to induce birth defects.
Tumor
[TOO-mur]
A mass of tissue characterized by thickness or volume.
U
Ultrasonography (Ultrasound)
[UL-trah-SO-nah-gra-fee]
The use of sound waves to examine the eye and orbit. Ultrasonography is commonly used to measure the size of tumors.
V
Vascular
[VAS-ku-lar]
Containing blood vessels.
Visual Field
[VIZ-yoo-ul FE-eld]
The complete area of vision that includes what is seen above, below, to the sides and in the center.
Vitreous
[VIT-tree-us]
The jelly-like substance which fills most of the normal eye.
Vitreous Seeding
[VIT-tree-us See-Ding]
Small pieces of tumor can break off “seed” and float around inside the eye.