25 Gauge Incision Anterior Segment Surgery Found Helpful For Both Tumor Biopsy: The Finger Iridectomy Technique
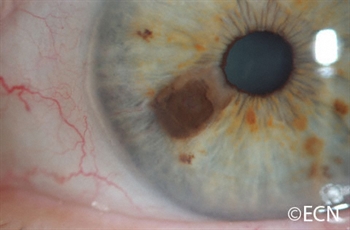
Iris, iridociliary, and other anterior segment tumors can be biopsied to help determine if they are a benign or malignant. In the past, a biopsy was either performed by aspiration through a needle [fine needle aspiration biopsy (FNAB)] or by a surgical iridectomy. The advantage of a needle biopsy was the very small “needle” incision that required no stitches or consequences for vision. Unfortunately, it was difficult to do more that scratch the tumor with the needle while aspirating a few cells. Using a sharp needle, the tumor often bleeds, clouding the view and making biopsy more difficult. In the past, the alternative was a surgical iridectomy that required a relatively large corneal incision, removal of a full-thickness piece of iris and sutures to close the corneal wound.
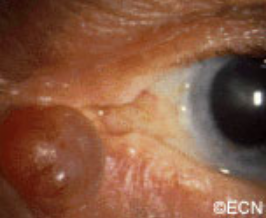
In an effort to make iris and ciliary body tumor biopsy safer and more effective, Dr. Finger invented a technique for minimally invasive iris biopsy (with less surgical trauma). This new technique combines the benefit of 1-mm typically sutureless incision with the ability to retrieve iris tumor biopsy specimens for pathology analysis. He has used this technique to perform tumor biopsy, iridotomy and to remove iris melanoma.
Dr. Finger has also used this technique to treat narrow angle glaucoma. Dr. Finger says, “it would be particularly useful for the treatment of children and mentally challenged adults who are not able to have the laser iridotomy method.” FIT can be used to surgically create a small hole in the iris through a 25 gauge self-sealing incision. “Micro-incision surgery should be safer for this group of patients who might rub their eye after surgery.”
For more information this technique has been recently published in the British Journal of Ophthalmology and Graefes Archive of Clinical and Experimental Ophthalmology.
The Finger iridectomy technique: small incision biopsy of anterior segment tumors.
Finger PT, Latkany P, Kurli M, Iacob C
The British Journal of Ophthalmology 2005;89:946-949
Small incision surgical iridotomy and iridectomy.
Finger PT.
Graefes Arch Clin Exp Ophthalmol. 2005 Aug 2;:1-2
The Finger Iridectomy Technique for Glaucoma
Finger PT
British Journal of Ophthalmology 2007;91:1089-1090.
Related Links
- Small Incision surgical iridotomy and iridectomy. Graefes Arch Clin Exp Ophthalmol. 2005 Aug 2;:1-2 [Epub ahead of print]
- A New Technique for 25-g Iridotomy, Iridectomy, and Tumor Biopsy – Retinal Physician
- The Finger Iridectomy Technique for Glaucoma – British Journal of Ophthalmology Abstract
- Search PubMed for 25 Gauge Incision Anterior Segment Surgery Found Helpful for Both Tumor Biopsy and Narrow Angle Glaucoma
- Search Google for 25 Gauge Incision Anterior Segment Surgery Found Helpful for Both Tumor Biopsy and Narrow Angle Glaucoma
Amniotic Membrane Is Used To Protect The Cornea During Plaque Radiation Therapy
By Paul T. Finger, MD
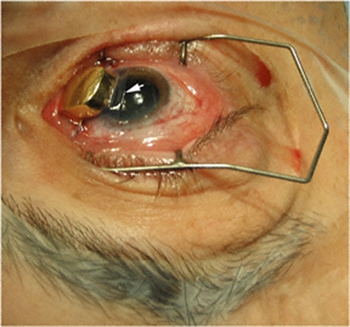
Patients with melanomas of the iris and ciliary body are more and more commonly treated with plaque radiation therapy. This is because I found radiation to be less invasive and therefore safer than intraocular surgery. Plus, larger areas can be treated with radiation than can be safely removed. This has allowed for excellent local control (tumor destruction) and vision retention. Though many irradiated patients develop radiation cataracts, these can be removed (the same way as other cataracts) restoring excellent vision. At The New York Eye Cancer Center, almost no patients with anterior intraocular melanomas have developed sight-limiting radiation maculopathy or optic neuropathy.
However, in the past, there have been problems associated with placing the radioactive plaque onto the cornea. First, there were concerns about irradiating the cornea. Second, many patients found having a metal device sewn to their cornea for 4-7 days painful.
Dr. Finger has found the cornea tolerated the amount of radiation required to treat iris and ciliary body melanomas. It remained clear for the vast majority of patients. However, having a radiation plaque sewn to the cornea was an uncomfortable procedure.
In an effort to solve this problem, Dr. Finger discovered that a thin, transplanted amniotic membrane tissue could be placed between the gold radiation eye plaque and the cornea during treatment. He simply slides this tissue between the plaque and the cornea during implantation. It is removed 7 days later when the plaque is removed. This technique has made a huge difference – it improved patient comfort and does not affect the radiation treatment.
This note is linked to a You-Tube video demonstrating this new technique. It shows implantation of a plaque onto the cornea and eye wall.
Related Links
- Watch YouTube video of actual “Finger’s Amniotic Membrane Graft Technique” surgery.
- Plaque radiation therapy for malignant melanoma of the iris and ciliary body – American Journal of Ophthalmology
- Tumour location affects the incidence of cataract and retinopathy after ophthalmic plaque radiation therapy – British Journal of Ophthalmology
- Search PubMed for Amniotic Membrane is Used to Protect the Cornea During Plaque Radiation Therapy
- Search Google for Amniotic Membrane is Used to Protect the Cornea During Plaque Radiation Therapy
Whole Body FDG – PET / CT: Imaging Cancer
By Paul T. Finger, MD
Whole body PET/CT technology combines positron emission tomography (PET) with computed radiographic imaging (CT) to put FUNCTION and FORM on the same diagnostic page (PET/CT).
Spiral computed tomography CT is used to generate anatomic images of the entire body. When suspicious areas or tumors are found, CT allows your doctor to see their size, shape and internal radiographic density. Though computed radiographic tomography (and magnetic resonance imaging – MRI) are excellent methods to determine if an abnormality exists, its shape and location, it cannot reveal if the abnormality (e.g. tumor, lesion) is metabolically active.
In contrast, Positron Emission Tomography (PET) is used to determine if tissues or tumors are metabolically active. This is important, because metabolically active tumors are more likely to be malignant. In the case of imaging of malignant melanoma, PET imaging can differentiate between benign cysts and metastatic tumors in the liver (and other sites). PET requires a small injection of radioactive material (e.g. FDG – radioactive glucose) that is preferentially absorbed by malignant tumors. It is important to note that any glucose absorbing process (inflammations, infections, working muscles and excretory systems) will also concentrate glucose and appear as a “hot-spot” on PET. However, PET does not give you shape or location. That is why and additional CT is needed. It is the addition of the anatomic information provided by CT that allows the physician to differentiate between benign and malignant tumors. The PET/CT computers unify the PET information over the CT information, placing form and function on the same diagnostic page.
Dr. Finger has shown the though the liver is the most common initial site of metastatic choroidal melanoma. It can occur in the bones (in 50% of cases). Clearly, a whole-body PET/CT scan from the top of the head to the bottom of the feet will include all the bones in the body. It is important to realized that not all metastases will “light-up” with PET and that sometimes a dedicated CT or MRI will offer better anatomic imaging. So don’t be surprised if there is suspicious area seen on PET/CT, your doctor may request an additional radiographic examination.
We expect more melanoma specific radioactive materials (other than FDG – radioactive glucose) to be used for PET/CT. This will improve the specificity and sensitivity of this test. To see the research work being conducted thus far, visit the links below.
Related Links
- An article on the use of PET/CT SUV as a biomarker for the risk of metastasis from choroidal melanoma
- The use of PET/CT for initial staging of choroidal melanoma
- The use of PET/CT to evaluate intraocular choroidal melanoma
- The use of PET/CT for patients suspected to have metastatic choroidal melanoma
- Search PubMed for Whole Body FDG- PET / CT
- Search Google for Whole Body FDG- PET / CT
3-Dimensional Ultrasonography
By Paul T. Finger, MD
3D ultrasound has been used to image radioactive eye-plaques while they are sewn beneath their intraocular tumors. This technique was used to make sure radioactive eye plaques are properly positioned beneath its intraocular tumor.
3D ultrasound is particularly helpful when examining eyes with tumors, retinal detachment and calcifications (e.g. retinoblastoma). It is a relatively inexpensive way to measure the diameter of the orbital portion of the optic nerve.
References
Finger PT, Romero JM, Rosen RB, Iezzi R, Emery R, Berson A. Three-dimensional ultrasonography of choroidal melanoma.Localization of ophthalmic plaques. The Archives Ophthalmology 116:305-12, 1998.
Related Links
Glossary
A
Adnexa
[Add-Nex-ah]
Appendages. Structures around the eye that support and surround it (e.g. the eye lids).
Alopecia
[Ah-lo-pee-Sh-ah]
Loss of body hair.
Alternative Treatment
Treatment other than the standard or most common treatment of a condition.
Anesthesia
[Ann-es-Thee-zee-ah]
Absence of normal sensation, usually a drug-induced decreased sensitivity to pain.
Apoptosis
[A-pop-Toh-sis]
A form of cell death where a programmed sequence of events leads to the elimination of cells without releasing harmful substances into the surrounding area.
B
Benefit
[Ben-eh-Fit]
The possibility of improvement (e.g., saving sight and saving life) by use of a diagnostic method or treatment.
Benign
[bee-NI-en]
The tendency to stay the same and not spread to other parts of the body.
Bias
[Bye-ass]
Personal preference not based on facts.
Biopsy
[Bye-op-see]
The removal of tissue, cells or fluids from the body for examination or study.
Brachytherapy
[Bray-key-THER-uh-pee]
Implanted radiation. For example, radiation treatment delivered by a small plaque sewn to the outside of the eye (sclera).
C
Cancer
[Can-sir]
A general term for more than 100 diseases characterized by an abnormal uncontrolled growth of cells. Cancerous tumors can invade and destroy surrounding normal tissues and/or spread to other parts of the body.
CAT Scan (aka computed axial tomography)
[KAT SKann]
An x-ray technique that uses computerized reconstruction to form an image of the inside of the body (head, orbit, chest, abdomen).
Chemotherapy
[KEY-mo-THER-uh-pee]
The use of topical or systemic drugs to treat cancer.
Choroid
[KO-royd]
Layer of normal blood vessels [vascular-layer] of the wall of the eye. The choroid is located between the retina and the sclera.
Choroidal Melanoma
[Ko-ROY-dull Mel-uh-NO-muh]
A malignant tumor (cancer) of the vascular “choroidal” layer of the eye, made up of pigment producing cells (melanocytes).
Chromosome 13
[Kro-moh-Some 13]
The piece of DNA that is responsible for the development of retinoblastoma.
Ciliary Body
[Silly-Airy Body]
An organ located right behind and encircling the iris. Tumors can come from the vascular and non-vascular parts of the ciliary body. The ciliary body also makes fluid which fills the eye.
Clinical Trial
[Klin-ick-al Try-ul]
The systematic investigation of the effects of specific treatments according to a formal research plan.
Complication
[Kom-plick-A-shun]
Undesirable effect of a disease or its treatment that can change the outcome and may require additional treatment.
COMS
Collaborative Ocular Melanoma Study. The largest prospective randomized clinical trial conducted to investigate choroidal melanoma.
Conjunctiva
[Con-junk-Tie-Vah]
A thin membrane that covers most of the outside of the eyeball and inside the eyelids.
Conjunctivitis
[Con-junk-Ti-Vie-tiss]
Inflammation or infection of the thin membrane that covers most of the outside of the eyeball and inside the eyelids.
Cornea
[KOR-nee-uh]
The clear outer portion of the eye which covers the iris and admits light through the pupil.
Cryotherapy
[KRY-oh-THER-uh-pee]
The destruction of tissue or tumor by the application of extreme cold.
Cyclotron
[SY-klo-tron]
A machine which creates high-energy radiation beams.
D
Depth Perception
The ability to recognize 3-dimensional objects and their relative positions in space.
Diagnosis
[dye-egg-NO-sis]
The name of a disease or condition.
Dormant
[DOR-mant]
A relatively inactive or resting condition in which some processes are slowed down or suspended.
Dosimetry
[Doe-si-met-tree]
The act of calculating the amount of treatment (e.g. radiation).
E
Enucleation
[e-noo-klee-AY-shun]
Removal of the eyeball, leaving the eye-muscles and other contents of the eye socket.
Equator
[EE-KWAY-Tore]
A circular position that divides the front from the back portion of the eye.
Eye Wall Resection
[eye-wall ree-SECK-shun]
Removal of the portion of the eye that contains the tumor.
F
Fluorescein Angiography
[FLOR-uh-seen an-jee-OG-ruh-fee]
A test where a vegetable dye is injected into a vein, allowed to circulate within the eye while photographs of the intraocular circulation are recorded.
Fovea
[Foe-Vee-ah]
The center of the macular retina primarily responsible for both color vision and fine resolution (reading vision).
G
General Anesthesia
[JEN-er-ruhl ann-es-THEE-zee-ah]
A complete drug-induced absence of sensation and consciousness induced by an anesthesiologist during surgery.
H
Hemangioma
[Hee-Man-gee-Oh-Ma]
Congental or acquired tumor comprised of blood vessels.
Hemorrhage
[HEM-or-ridge]
Loss of blood, either inside or outside the body.
I
Implant
[Im-Plant]
A device which is placed inside. For example, an implant is placed into the orbit to make up for the loss of the eyeball during enucleation surgery.
Informed Consent
[In-formd Kon-sent]
The process where a patient learns about all the aspects of a medical treatment or clinical trial before agreeing to participate. This process should include a detailed explanation of the potential risks and benefits of all standard medical procedures and treatments.
Interferon
[In-ter-Fear-on]
A immune system modulator used to treat conjunctival and corneal cancers. This chemotherapy drug is either used as an eye drop and/or injected around the tumor.
Iodine-125 Seeds
[I-O-dine 125 seeds]
Rice-sized radioactive sources which are typically purchased and glued within gold eye-plaques for use in treatment of intraocular tumors.
IRB
[Institutional Review Board]
A committee of people who typically reviews, approves or denies the right to conduct a scientific study. IRB’s assure that such studies are ethically and scientifically proper.
Irradiate
[ear-Ray-dee-ate]
To expose part of the body to diagnostic or therapeutic radiation.
J
Juxtafoveal
[Jux-Tah-Foe-Ve-al]
Located next to (touching) the fovea.
Juxtapapillary
[Jux-Tah-pap-hill-airy]
Located next to (touching) the optic nerve.
K
Keratitis
[Ker-ah-tie-tis]
Irritation or inflammation of the cornea. Keratitis can be due to exposure, radiation, infection, or immune reaction.
L
Laser
[LAY-zur]
A very narrow, high intensity, light, which can burn tissue and/or join structures together.
Lens
[Lenz]
A clear structure behind the pupil, which helps to focus light onto the retina.
Local Anesthesia
[LOW-cull ann-es-THEE-zee-ah]
The patient is awake but drugs have been given to decrease or stop sensation in the area of surgery.
Lymphangiectasia
[limf-an-gee-eck-tae-Z-ah]
A dilated lymphatic channel, commonly filled with blood.
M
Macula
[Mack-U-Lah]
The part of the retina responsible for the center of vision.
Malignant
[ma-LIG-nant]
When a tumor contains cancer cells that can spread and cause death.
Melanoma
[mel-uh-NO-muh]
A tumor made up of pigment cells called melanocytes.
Metastasis
[meh-TASS-tah-sis]
The site where the cancer cells have spread to form a tumor.
Metastasize
[me-TAS-tah-size]
The spread of cancer cells from the original tumor to a distant site.
Mitomycin
[My-toe-My-cin]
A chemotherapy drug sometimes used to treat conjunctival and corneal cancers.
Mitosis [Mitotic]
[My-Toe-Sis]
The process when the cell (and its chromosomes) divides.
N
Neovascularization
[Nee-Oh-Vas-Q-lar-eye-zay-shun]
The growth of new blood vessels into, around or within tissue.
O
Ocular
[ock-yu-lar]
Of or pertaining to the eye.
Ocularist
[ock-u-lah-rist]
A specialist who makes and fits artificial eyes.
OD [oculus dexter]
Latin for “right eye.”
Oncologist
[ON-kol-oh-gist]
A general medical doctor who specializes in cancer treatment.
Ophthalmic Oncologist
[off-thal-mick ON-kol-oh-gist]
An ophthalmologist with special training in the diagnosis and management of patients with eye cancer.
Ophthalmologist
[off-thal-mol-loh-gist]
A physician with special training in the medical and surgical treatment of eye diseases.
Optical Coherence Tomography (OCT)
[Op-tic-al Coh-hear-ents Toe-Mah-Graph-E]
Where a laser imaging device is used to image the eye. It can be used to image the front of the eye, but for eye cancers it is most commonly used to observe the retina, choroid and sclera.
Optic Nerve
[OP-tick nurv]
The nerve that sends vision-messages between the brain and the eye.
Optic Neuropathy
[OP-tick nur-Op-ath-he]
Used to describe when the optic nerve appears or functions abnormally.
Orange Pigment
Collections of lipofuscin pigment typically seen on the surface of choroidal melanomas or suspicous choroidal nevi.
Orbital Tumor
[oar-bit-tall TOO-mur]
A benign or malignant tumor behind or around the eye.
OS [oculus sinister]
Latin for “left eye.”
OU [oculus uterque]
Both eyes.
P
Palladium-103 Seeds
[pah-lay-dee-um 103 seeds]
Rice-sized radioactive sources which are typically purchased and glued within gold eye-plaques for use in treatment of intraocular tumors.
PET / CT
[Pah-Zit-tron EE-miss-shun Toe-mog-graph-Fee / Cat-skah-hun]
An imaging study that can provide images of the whole body looking for evidence of cancer.
Photocoagulation
[Foe-Toe-Koe-ah-gu-LAY-shun]
The use of intense light (usually laser-beams) to destroy eye tissues, abnormal blood vessels, and/or tumors.
Pigmentation
[PIG-men-tay-shun]
The color of the body.
Pigmented Cells
[PIG-men-ted sells]
Cells, which are colored and usually contain the natural pigment of the skin or eye, called melanin.
Plaque
[plak]
A bowl-shaped device, which is, or can be made radioactive by adding seeds. An ophthalmic plaque is typically sewn to the wall of the eye in order to treat an underlying intraocular tumor. Plaque therapy is the most common treatment for choroidal melanoma.
Primary Cancer
[PRY-may-ree Kan-ser]
The original malignant tumor from which cells can spread to other parts of the body.
Prognosis
[Prog-NO-sis]
What is most likely to happen over time.
Proptosis
[Prop-Toe-Sis]
When the eye is (displaced) pushed forward from its normal position.
Prosthesis
[pross-thee-sis]
A device that is used to replace the appearance and/or function of a removed organ. For example, the plastic eye that is placed beneath the eyelids to simulate a removed eye.
Proton Beam Radiation
[prote-on beem ray-dee-ay-shun]
Radiation made up of protons, which come out of a machine, travel through the eye into the tumor.
Pupil
[pyoo-pill]
The round opening in the iris which lets light into the eye and onto the retina.
R
Radiation
[ray-dee-Ay-shun]
Energy waves which can be used to diagnose (e.g. chest x-rays) or treat diseases (e.g cancers).
Radiation Oncologist
[ray-dee-AY-shun ON-kol-OH-jist]
A physician with special training in the use of radiation to treat diseases.
Radiation Retinopathy
[ray-dee-Ay-shun RET-in-opp-ah-thee]
When large amounts of radiation cause vascular changes in the normal retina often resulting in decreased vision.
Radiation Therapy
[ray-dee-AY-shun THER-ah-pee]
The use of high-energy radiation to treat cancer and certain benign diseases.
Radioactive Plaque
[ray-dee-OH-ack-tiv plak]
A bowl-shaped radiation device which can be used to treat eye cancers (e.g. melanomas and retinoblastomas).
Randomization
[RAN-dum-eye-ZAY-shun]
The process of assigning patients to two or more treatment options, where each patient has an equal chance of receiving each treatment.
Retina
[REH-tin-uh]
The nerve tissue which lines the inside of the eye and acts like the film inside a camera.
Retinoblastoma
[Ret-in-OH-blast-OH-mah]
A cancerous tumor of the retina which typically affects children under 5 years of age. Retinoblastoma is the most common malignancy to start within the eye of children.
Risks
The possibility of loss or injury resulting from a condition or treatment.
S
Sclera
[SKLEHR-uh]
The white outer wall of the eye.
Scotoma
[SkoH-Toe-Mah]
A blind-spot or defect in the field of vision.
Side Effect
An unwanted effect of treatment.
Standard Treatment
The accepted, recognized and commonly used form of therapy. What is typically used by most physicians treating a particular disease.
Stereopsis
[Stay-re-op-sis]
The ability to see objects with depth perception from both eyes.
T
Teratogenic
[Tear-at-Oh-gen-ick]
The tendency to induce birth defects.
Tumor
[TOO-mur]
A mass of tissue characterized by thickness or volume.
U
Ultrasonography (Ultrasound)
[UL-trah-SO-nah-gra-fee]
The use of sound waves to examine the eye and orbit. Ultrasonography is commonly used to measure the size of tumors.
V
Vascular
[VAS-ku-lar]
Containing blood vessels.
Visual Field
[VIZ-yoo-ul FE-eld]
The complete area of vision that includes what is seen above, below, to the sides and in the center.
Vitreous
[VIT-tree-us]
The jelly-like substance which fills most of the normal eye.
Vitreous Seeding
[VIT-tree-us See-Ding]
Small pieces of tumor can break off “seed” and float around inside the eye.
Benign Eyelid Tumors – Nevus at the Eyelid Margin
By Paul T. Finger, MD
Description
A nevus (a benign tumor) is commonly found on the skin of other parts of the human body. A nevus can also occur on the eyelid skin. These tumors are usually pigmented and have thickness.
Symptoms

Patients typically notice a dark spot on their eyelid that is thickened. It usually does not cause loss of eyelashes and though it can grow, most do not. When rapid (over months) growth, loss of eyelashes or discoloration of the nevus is noted, malignant melanoma is suspected.
Diagnosis
Most eyelid nevi can be diagnosed by clinical examination. A baseline photograph should be obtained for comparison with future examinations. Very suspicious or rapidly growing eyelid nevi should be biopsied to rule out melanoma. It is important to note that eyelid nevi can slowly grow, and that change is particularly common during puberty.
Treatments
Eyelid nevi are benign tumors. They can be photographed and followed for evidence of change or growth prior to consideration of biopsy or treatment. Large eyelid nevi can be a cosmetic problem that can be repaired by ophthalmic plastic surgery.
Related links
Benign Eyelid Tumors – Hydrocystoma
By Paul T. Finger, MD
Description
The benign eyelid tumor hydrocystoma comes from the Latin hydro, meaning fluid, and cystoma, meaning cyst or sac.
A hydrocystic thickening is an epithelial-lined serous cyst (within the skin or soft tissues). Sometimes it looks like they are translucent.
Symptoms
Hydrocystomas most commonly occur on the eyelids. They typically are the same color as eyelid skin, rounded and soft to the touch. They are slow growing, may cause misdirection but not loss of eyelashes.
Diagnosis
Hydrocystoma is a benign tumor that can be photographed and followed for evidence of growth. High-frequency ultrasound can demonstrate that the tumor is filled with fluid and confirm the diagnosis.
Treatments
Excision is typically performed if growth is documented, basal cell or other eyelid cancer is suspected and for cosmetic reasons. During removal, your surgeon will try and keep the cyst intact. Removing the whole tumor will help keep it from recurring.
Related Links
Benign Eyelid Tumors – Capillary Hemangioma
By Paul T. Finger, MD
Description

Congenital “strawberry-spot” which usually will spontaneously get smaller “involute.”
Treatment is indicated for the prevention of amblyopia (loss of vision) and strabismus (misdirected eyes). These tumors naturally grow and then spontaneously decrease in size. Therefore, if the tumor is not harming the child, it can be observed untreated for spontaneous regression.
Symptoms
Capillary hemangiomas are typically found at birth. They will grow during the first decade (10 years) and most will shrink (involute). If they involve the eyelids, they can cover the eye and cause loss of vision (amblyopia). It is very important that children with capillary hemangiomas be seen by a pediatric ophthalmologist and eye cancer specialist immediately.
Diagnosis
Capillary hemangioma is diagnosed by clinical examination. It has a typical appearance and biopsy is rarely needed. It appears as a reddish tumor or mass beneath the skin. The eye care specialist will order a radiographic scan (MRI or CT) to see how deep the tumor extends into the orbit (around the eye). The child’s pediatrician should be advised and the child inspected for hemangiomas on other parts of the body.
Treatments
Observation for spontaneous resolution is commonly performed. If the tumor is blocking the eye and vision causing amblyopia, then it can be treated with an oral beta-blocker medication (e.g. propranolol) or injected with a steroid solution. This will shrink the tumor in an effort to uncover the eye. Surgery may be required to remove very large tumors. The child’s pediatric ophthalmologist may suggest that the other “good” eye be periodically covered with a patch to strengthen the tumor affected eye and prevent amblyopia-related vision loss.
Related Links
Basal Cell Carcinoma (Eyelid Cancer)
By Paul T. Finger, MD
Description

The most common type of eyelid cancer is basal cell carcinoma. Most basal cell carcinomas can be removed with surgery. However, many older patients will try to ignore these slow growing tumors. However, it is important to know that when left untreated, these tumors can grow around the eye and into the orbit, sinuses and brain. Basal cell carcinomas are more commonly found on the lower eyelids and almost never spread to other parts of the body (metastasize).
Symptoms
Patients with basal cell carcinomas most commonly notice a reddish nodule slowly forming on their eyelid. The tumor is most commonly found on the lower eyelid, followed by the medial canthus (skin toward the nose) and can occur on the upper eyelid. Eyelash loss (around the tumor) suggests that a basal cell carcinoma is malignant.
Less commonly, basal cell cancers can be pigmented or present without any nodule at all. When the tumor does not make a nodule and grows within the eyelid, it can induce pulling of the eyelid (away from the eye). Doctors call this form of basal cell carcinoma “morpheaform,” which are much more difficult to cure because its edges are harder to define.
Diagnosis
Though small tumors can be photographed and followed for evidence of growth (prior to biopsy); once your eye cancer specialist suspects basal cell carcinoma, most eye cancer specialists will suggest tumor biopsy. This specimen is sent to the pathologist to confirm the diagnosis prior to complete removal or treatment of the tumor. Biopsies can be performed in the doctor’s office, or in the operating room prior to definitive treatment.
Treatments
Once the diagnosis is confirmed by the pathologist, treatment will be recommended. Wedge resection and Moh’s surgery require the surgeon continue to remove the tumor until the margins (edges) are negative (free of tumor). Unlike most skin, the eyelid are a complex functional apparatus that requires special reconstruction techniques.
Most basal cell carcinomas are cured when they are small. Unfortunately, some patients choose to ignore or deny the existence of these tumors. Those patients allow their tumor to invade behind the eye and become difficult or impossible to remove. In these cases, combinations of surgery, radiation and chemotherapy may be required to control or destroy the tumor.
Additional Info
This is a sun related cancer. Dr. Finger suggests, “Think of sunglasses as sunblock for your eyes”™
Related Links
Search Recent Scientific Publications about Basal Cell Carcinoma of the Eyelids









