Periocular Hemangioma of Childhood
By Paul T. Finger, MD
Description

Children can either be born with or develop reddish “strawberry” colored tumors on or around their eyes. This is one of the most common tumors of infancy. It is 3 times as frequent in girls and can run in families.
Symptoms
Periocular hemangioma of childhood can be large, and commonly grow during the first year of life, but also tend to get smaller (involute) over the following 2 years.
Periocular hemangioma of childhood can extend into the orbit (behind the eye) and push the eye forward (proptosis), make the eyes misaligned (strabismus), or can cause the eyelid to droop (ptosis).
Children with periocular hemangioma of childhood can have hemangiomas in other parts of their bodies, so a pediatric consultation is necessary. If the hemangiomas are multiple or on the jaw or neck, a pulmonary consultation is necessary to rule out upper respiratory tract involvement. Consider the PHACES syndrome (anomalies of the Posterior fossa, Hemangiomas, the Arteries, Cardiac, Eye, Sternum) which is more commonly seen in girls.
Diagnosis
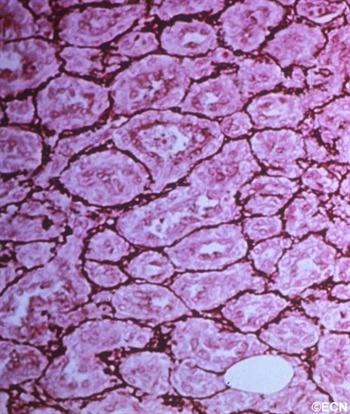
Hemangioma can be diagnosed by ocular examination with magnetic resonance imaging (MRI). Rarely, a small biopsy may be required to confirm the clinical diagnosis.
Treatments
Since periocular hemangioma of childhood is a benign tumor (not a cancer), immediate treatment is often not necessary. In fact, after an initial growth phase, many of these tumors will get smaller by themselves. Most patients can be followed for evidence of spontaneous remission.
Treatment is urgently indicated if the periocular hemangioma of childhood is found to harm the proper development of vision in the affected eye in infants and young children (amblyopia), and for psychosocial reasons in older children and adults.
Let me explain Amblyopia: In order for an eye to achieve its best possible potential for vision, two things are necessary. First, proper images must be focused on the retina and second, the brain must receive those images. During the first 10 years of life, there is a process where images are collected and the brain learns to understand those images. If an eye is blocked by the tumor (or the eye lid), or if the eyes are not aligned, or if the eye is not able to focus images on the retina, the child’s eye-brain connection will not develop. That is, the child will not learn to see from that eye (a problem called amblyopia). Urgent treatment of periocular hemangioma of childhood can be necessary be to prevent amblyopia.
Periocular hemangioma of childhood has been treated with surgery, laser-surgery, radiation, and drugs (intralesional steroids and systemic beta-blockers). When possible, treatment of periocular hemangiomas of childhood involves injections of steroid into the tumor. In comparison to taking the medicine by mouth (PO) or by vein (IV), this approach has the advantage of putting the medicine right into the tumor. An acute effect, but does carry risk of tumor and orbital hemorrhage.
References
- Haik B, Karcioglu Z, Gordon RA, Pechous BP. Capillary hemangioma (infantile periocular hemangioma). Survey of Ophthalmology 1994;38:399-426.
- Kushner BJ. Hemangiomas. Archives of Ophthalmology 2001;118;835-836.