International Multicenter Cooperative Study Supported by The Eye Cancer Foundation
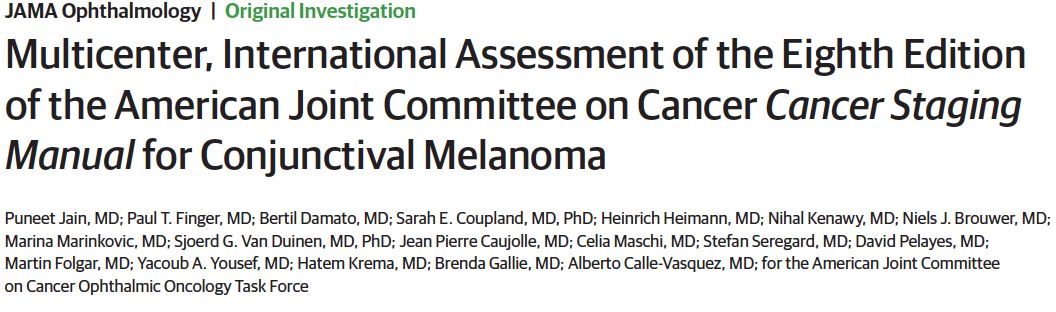
The American Joint Committee on Cancer (AJCC) Cancer Staging Manual compiles all currently available knowledge on cancer staging at various anatomic sites. In 2016, they released the 8th edition, conjunctival melanoma staging system which features 12 new staging systems, a wide range of new staging definitions, and an emphasis on the personalized-medicine approach. This staging system is used and respected by medical, ophthalmic, and radiation oncologists because it standardizes data reporting, prognosis, and selection of the best treatment for conjunctival melanoma. Nonetheless, a collaborative multicenter international registry was organized by our very own Dr. Finger to evaluate the accuracy of such a staging system. In addition to the 19 co-authors listed, Dr. Puneet Jain led the analysis, writing and collaborative revision of this study. He completed an Eye Cancer Foundation-sponsored Fellowship. ECF fellowships are known to foster ophthalmic oncology training, curiosity, learning and ability to perform research!
This study, performs the first ever international multicenter study to evaluate the validity of the eighth edition of the American Joint Committee on Cancer (AJCC) Cancer Staging Manual in estimating mortality rates of metastasis from conjunctival melanoma. The 8th edition AJCC ophthalmic oncology staging systems were written by more than 50 eye cancer specialists from 18 countries.
In this study, co-investigators utilized internet-based data sharing, reviewing 288 conjunctival melanoma patient medical histories. This study included data from 10 ophthalmic oncology centers in 9 countries over 4 continents — 2 in the United States and 1 in Canada, Colombia, Argentina, France, Netherlands, United Kingdom, Sweden, and Jordan. Clinical (cT) and pathologic (pT) staging were performed according to the staging system for conjunctival melanoma in the 8th edition of the AJCC Cancer Staging Manual.
This study was able to find new insights by conducting an analysis of large numbers of rare tumors. The findings corroborate the validity of the 8th edition of the AJCC Cancer Staging Manual. However, it also found several independent factors that are associated with increased mortality, such as tumor thickness, tumor invasion, and ulceration. Ultimately, this study supported the continued use of conjunctival melanoma staging system as published in the 8th edition of the AJCC Cancer Staging Manual.









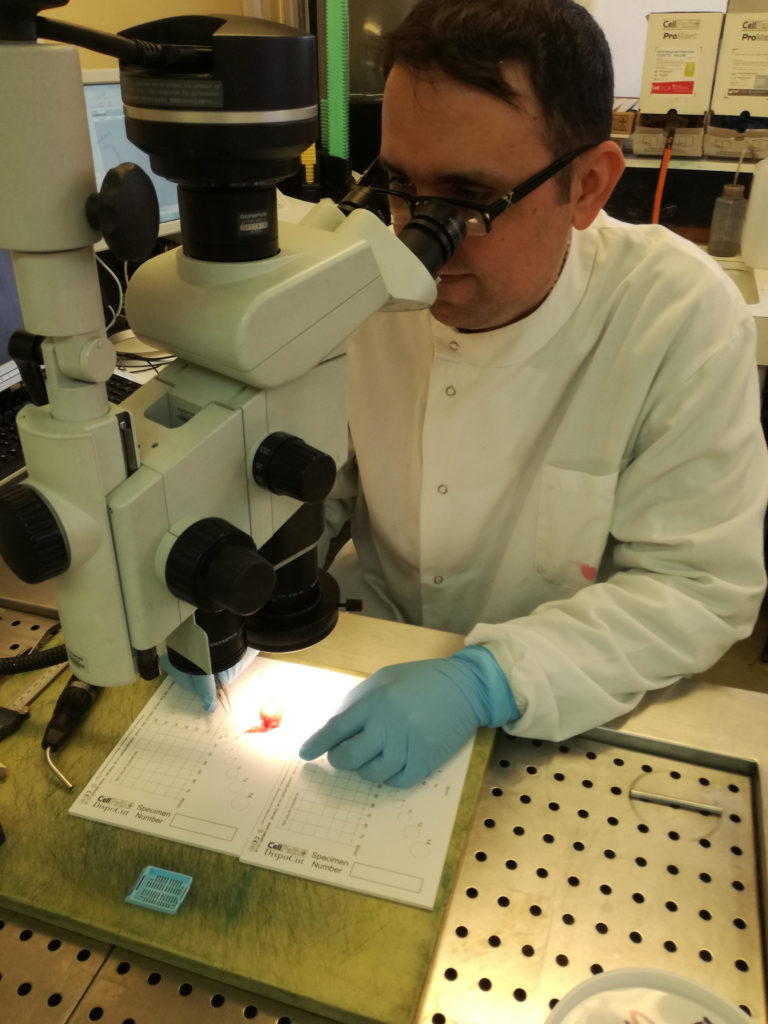
 Prior to involvement of The Eye Cancer Foundation (ECF), Jordan had no practicing eye cancer specialists. We trained Dr. Yacoub Yousef and he established the first eye cancer referral center at The King Hussein Cancer Center in Amman. After years of building this center, Dr. Yousef has trained many eye cancer specialists for the surrounding countries and has offered life and vision-sparing treatments for patients throughout the Middle East. Finally, with a place to go, patients requiring eye treatment inundated these hospitals. With more and more patients needing eye cancer services, Jordan and the Middle East needed a specialist in eye pathology.
Prior to involvement of The Eye Cancer Foundation (ECF), Jordan had no practicing eye cancer specialists. We trained Dr. Yacoub Yousef and he established the first eye cancer referral center at The King Hussein Cancer Center in Amman. After years of building this center, Dr. Yousef has trained many eye cancer specialists for the surrounding countries and has offered life and vision-sparing treatments for patients throughout the Middle East. Finally, with a place to go, patients requiring eye treatment inundated these hospitals. With more and more patients needing eye cancer services, Jordan and the Middle East needed a specialist in eye pathology.