Case #3: Choroidal Hemorrhage
By Paul T. Finger, MD
History
An 80-year-old male with a past history of coronary artery disease,and cataracts (removed in 1986 and 1996). He has been taking aspirin and Vitamin E for several months, but had discontinued both due to ecchymosis on both hands.
He was referred to The New York Eye Cancer Center for an evaluation of an intraocular tumor and 2 weeks of ocular pain with photophobia OD.
Ophthalmic examination revealed a visual acuity of 20/25 OU. His pupils were asymmetric (without APD) and his visual fields were restricted OD, full OS. Ocular motility was within normal limits.
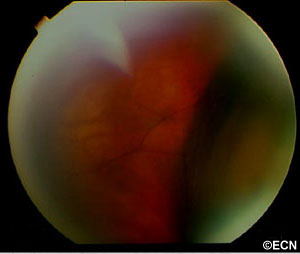
Intraocular pressure measurements were 13 OD and 11 OS. Slit lamp biomicroscopy revealed posterior chamber implants with some retained cortical material in the superotemporal quadrant OD. There is no tumor in the angle on gonioscopy and no mass effect on the iris. Both high frequency and low frequency ultrasonography were performed:
A 2-dimensional 10 MHz transocular ultrasound at the plane of the equator-anterior meridian revealed a multilobular thickening of the anterior choroid with variably reflective subretinal echoes. On dynamic ultrasound examination of the retina, it was found to undulate with eye movement (consistent with hemorrhagic choroidals). A-scan was used to evaluate the subretinal material. It was found to be completely echolucent (ARROW) at 67 db consistent with blood or (less-likely) exudative fluid.
Impression
Spontaneous Hemorrhagic Choroidals
Recommendations
Dr. Finger’s primary recommendation was serial observation. There was a small possibility of a hemorrhagic neoplasm beneath the choroidals or a ring melanoma. With this in mind, the patient was given a complete metastatic survey as well as evaluations for coagulopathy. He was advised not to lift, strain, or rub his eye, that he should use Tylenol instead of aspirin, and not use his Vitamin E supplements. He was warned that should the blood dissect into his macula, this may result in some level of permanent (unilateral) loss of vision. He was to continue taking Advil for pain control. One month later, along with his pain the choroidals were largely resolved. His vision continued to be 20/25 OU.
Related Links
Case #2: Necrotic Choroidal Melanoma
By Paul T. Finger, MD
History
A 55-year old female presented to The New York Eye Cancer Center with swelling of her eyelids, signs of scleritis, and pain on eye movement. Her visual acuity was correctable to 20/20 OU, and ophthalmoscopy was significant for a hemorrhagic chorioretinal thickening in the superotemporal quadrant.
Fundus photographs and a Fluorescein angiogram were obtained utilizing Digital Photography (see right).
3D-Ultrasonography is significant for a 13 x 13 mm (base), 5.0 mm height choroidal tumor with moderate internal reflectivity. The tumor’s surface is irregularly shaped, the subjacent sclera was thickened, and a retrobulbar lucency “edema” is evident. However, there was no extrascleral tumor extension.
Fluorescein angiography reveals a small patch of intraretinal microangiopathy, leaking retinal vessels, and diffuse areas of blockage.
The differential includes infectious, inflammatory, neovascular, and neoplastic events. When all testing proved negative our options included biopsy or close serial observation.
3 Months after Initial Presentation
A fundus photograph (see right) reveals a marked reduction of subretinal fluid and hemorrhage. Exudates have appeared at the infero-temporal margin, and orange pigment on the inferonasal tumor.
| Serial Ultrasound Evaluations | ||||
| Variable | Presentation | 2 months | 3 months | 5 months |
| Tumor Height | 5.0 mm | 4.0 mm | 1.9 mm | 3.2 mm |
| Reflectivity | Medium | Medium | Variable | Low |
| Surface | Irregular | Irregular | Concave | Dome |
Impression
Necrotic Choroidal Melanoma
This is an atypical presentation for choroidal melanoma. In this case serial observation over time allowed for clearing of the overlying blood and serous fluid. We were eventually able to view of the tumor’s surface (e.g. orange pigment). Serial ultrasonography demonstrated both resolution of the inflammatory and hemorrhagic components, shrinkage, and finally evidence of growth.
In this case, close observation (together with a careful medical work-up) allowed the choroidal melanoma to evolve into a more recognizable form and to demonstrate its tendency to grow.
Recommendation

Ophthalmic Plaque Radiation Therapy
The risks and benefits of continued observation for growth, enucleation, radiation therapy (both proton versus plaque), as well as currently available alternative therapies were discussed in detail. After a discussion of the comparative dosimetric advantages of palladium-103 versus iodine-125 plaque radiation therapy, she chose palladium-103 as treatment for her choroidal melanoma.
Related Links
Case #1: Iris Melanoma or Iris Melanocytoma?
By Paul T. Finger, MD
History
A 32 year old male presented with “two pupils” in his left eye. He had been noted to have had multiple episodes of blurred vision and discomfort from his left eye.
Digital photography with gonioscopy was obtained.
His intraocular pressure was elevated to 32 mm Hg OS and gonioscopy revealed pigment dispersion for 360 degrees. As demonstrated below, high frequency ultrasound was performed.
Impression
Melanomalytic glaucoma
This patient’s primary problem is his glaucoma as the rate of metastasis in iris melanomas has been found to be low (1-5%). This particular tumor demonstrates two reasons why the risk of metastasis is low in these cases. First, it is small (largest diameter = 2.3 mm). Second, the tumor is far from the ciliary body and other routes of tumor dissemination. Risk factors for metastasis in iris melanoma include: large tumor size, ciliary body invasion, pigment dispersion, secondary glaucoma and extraocular extension of tumor.
In this case his glaucoma has been controlled with topical medication. Eventually he may require laser trabeculoplasty or cyclophotocoagulation. I do not recommend filtering surgery in these patients. Though not proven as a risk factor, filtering surgery clearly allows egress of melanoma cells into the orbit (as does extraocular extension).
Recommendation
Iridectomy
A transcorneal surgical iridectomy or FIT should be considered. It would remove the tumor, the source of pigment/cells, and the cause of the glaucoma.
There has been considerable controversy as to whether suspicious iris melanotic lesions should be removed. Without secondary glaucoma resectable iris melanomas are typically watched for evidence of growth prior to resection.
In this case, he already has a visual field defect and his tumor is the source of his pigmentary glaucoma (a risk factor).









