Sebaceous Carcinoma of the Eyelid
By Paul T. Finger, MD
Description
Sebaceous carcinoma arises from the glands within the eyelids, caruncle or eyebrow. They are more commonly found on the upper eyelid and in middle-aged patients.
Symptoms

Sebaceous carcinomas are one of the rarest eye cancers and can look like a chalazion (stye) or conjunctivits. In that sebaceous carcinoma can mimick these relatively benign dieases, eye care specialists should be suspicious of this tumor in any patient with persistent conjunctivitis, blepharoconjunctivitis or chronic/recurrent chalazion. Therefore, any conjunctivitis or chalazion that is not getting better after 3 months of observation, should be biopsied.
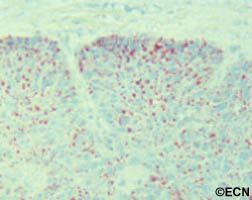
Diagnosis
Sebaceous carcinoma of the eyelid typically presents as a yellow-nodule in the upper lid. The patient may have history of colon, breast, genitourinary or other skin malignancies (Muir-Torre Syndrome).* When a nodular tumor, it can cause eyelash loss, but is not painful (compared to styes). This tumor can also present as a hypervascular conjunctival tumor and tends to spread along the conjunctival surface. In these cases sebaceous carcinoma looks like conjunctivitis.
It is worth repeating that “any conjunctivitis or chalazion that is not getting better after 3 months of observation should be biopsied.” If cytopathology is available at your medical center, a scrape biopsy of the conjunctiva can be initially performed in the office setting. However, the gold standard for diagnosis of sebaceous carcinoma is histopathologic evaluation of a fresh tissue specimen.
Once the diagnosis is made, a metastatic survey is warranted. Sebaceous carcinoma can spread to regional lymph nodes (pre-auricular and cervical) as well as to lungs, brain, liver and bone. At The New York Eye Cancer Center, we obtain a total body PET/CT scan (from head to toes) for staging. Published series have reported that the occurrence of metastatic disease was dependent on the size and location of the primary tumor and occurred in up to 27% of patients. Local tumor invasion of the lymph nodes, orbit or metastatic sites were associated with a poor prognosis for survival.
Treatments
Treatment requires a resection of the malignancy. Frozen section control can be used to provide negative margins. Larger surgeries, cryodestruction and radiation may be required if resection is not possible. Exenteration (complete removal of the orbital contents is sometimes required for extensive or recurrent disease).
* Muir-Torre Syndrome: A rare, genetically autosomal dominant cancer syndrome. Patients with Muir-Torre can develop cancer of the colon, breast, genitourinary tract, skin and eye lesions, including keratoacanthomas and sebaceous carcinoma.









