2020 Fellowship
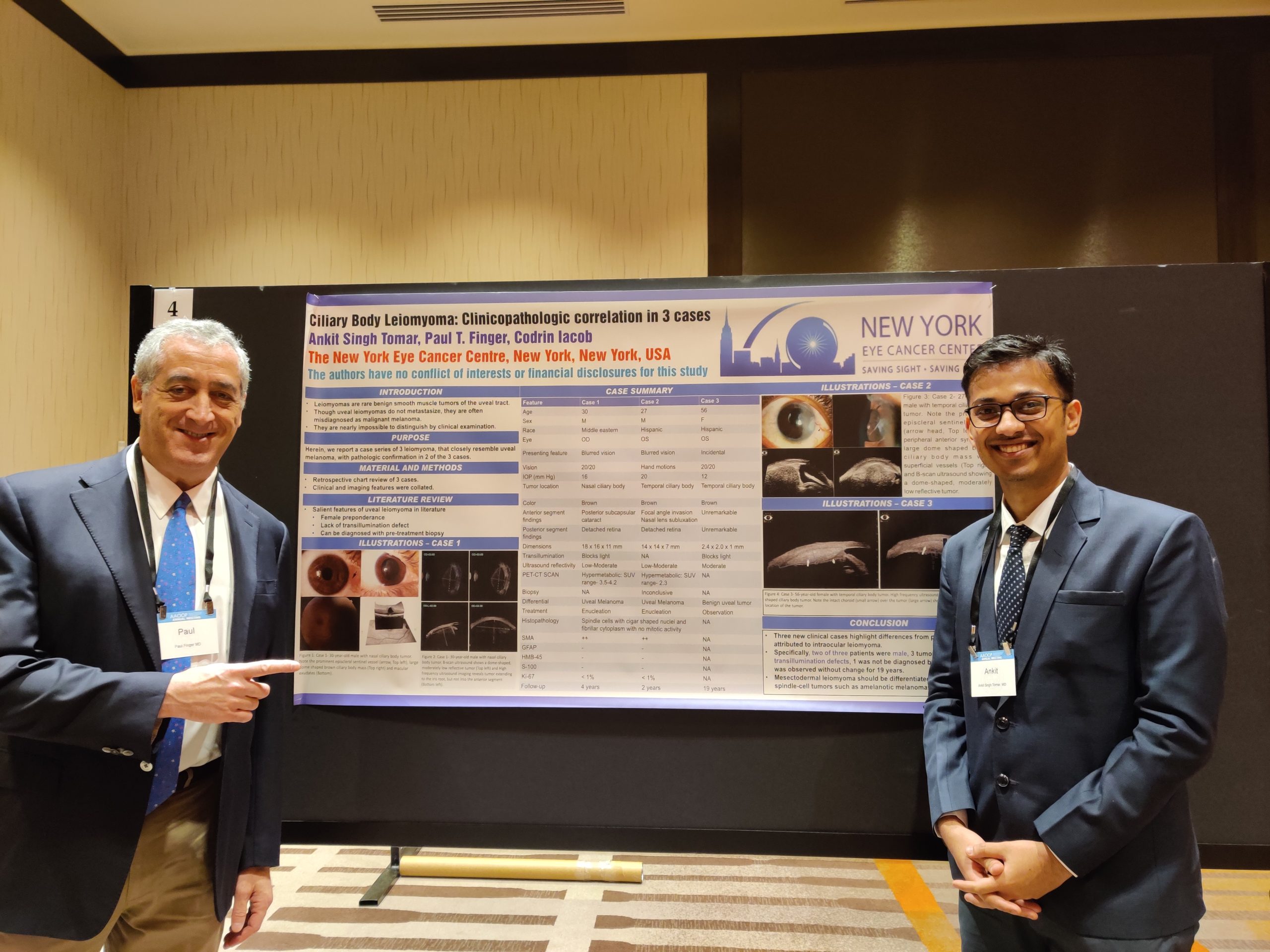
Ghana is another country claimed by the Eye Cancer Foundation! Recently, Dr. Akosua Boateng finished her training sponsored by The Eye Cancer Foundation (http://eyecancercure.com). She notes, “I have always been interested in ocular pathology, but had never truly had the opportunity to nurture the interest due to a lack of resources in my home country.” However, she was awarded the opportunity to train in ophthalmic pathology with an emphasis on retinoblastoma at the Beijing Children’s Hospital due to a joint effort of Dr. Paul Finger of The Eye Cancer Foundation and Dr. Brenda Gallie of the University Health Network, Princess Margaret Cancer Center of Toronto.
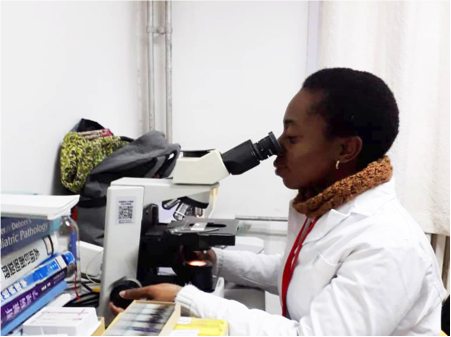
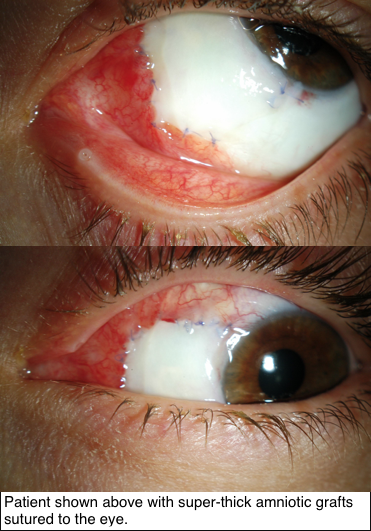
Dr. Boateng was determined to learn about the clinical presentation, examination, and treatment for many ocular cancers as well as be able to recognize their pathology on slides under the microscope. Her training
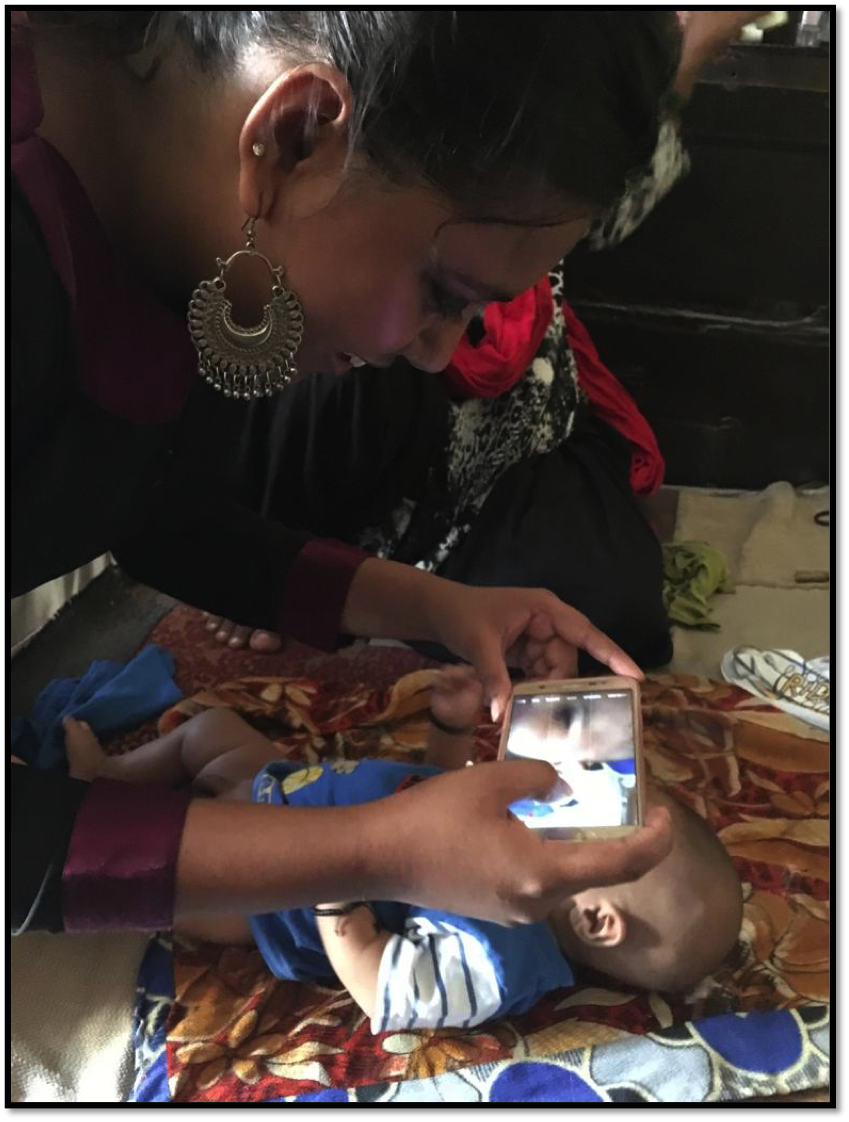
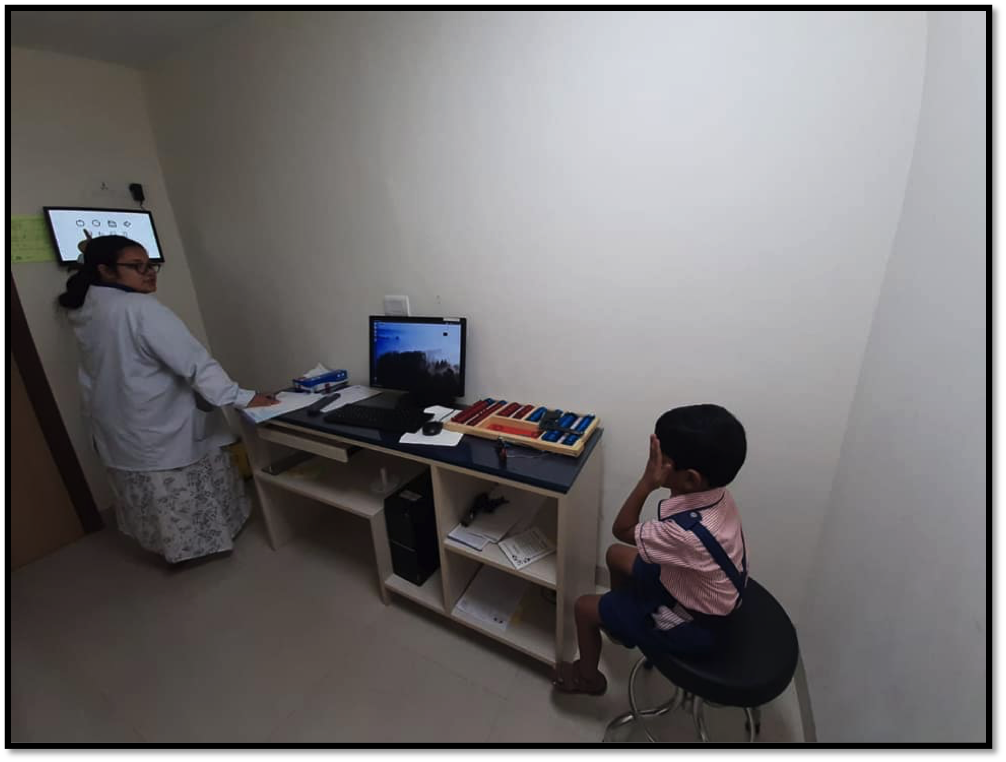
was split between a clinic with Dr. Jeffrey Zhang, retinoblastoma care with Dr. John Zhao and the pathology department with Dr. Nan Zhang. During clinic days, Dr. Boateng learned about many eye diseases including myopia, congenital anophthalmia and others. For the first time, she learned how to perform intraocular photography with the Retcam Imaging System. For retinoblastoma care, Dr. Boateng was able to examine the fundus of both old, treated and new cases. She took part in discussions of the children’s treatment options. She spent time in the operating theatre shadowing surgeries, such as laser treatment, chemotherapy and enucleation. She learned to differentiate between retinoblastoma and Coat’s Disease. In the pathology department, first she learned more about the anatomy of the eye, identified histologic high-risk factors for retinoblastoma, and how to stage cases according to the AJCC 8th Edition Manual. She says it was a “great learning experience.”.

Unfortunately, due to the Covid-19 pandemic, Dr. Boateng was forced to abruptly end her training months prior to completion. Thus, she would like to return to learn more about adult ocular pathology as it would be helpful back in Ghana. However, when Dr. Boateng returned to her parent hospital in Ghana, she feels so much more confident in dealing with ocular pathology and retinoblastoma. She is grateful to Drs. Finger and Gallie as well as The Eye Cancer Foundation for allowing her intensive training to happen!