Focusing on Childhood Eye Cancer Awareness
Through the month of September, families, caregivers, charities, and researchers across the country observed Childhood Cancer Awareness Month. Cancer is the leading cause of death by disease in children under the age of 15. In the US alone, more than 15,000 children are diagnosed with cancer every year. While Leukemia and brain tumors are the most common cancers in children and get the most attention, eye cancer also affects kids.
Retinoblastoma is the most common intraocular cancer in young children. It typically develops by the age of five and affects approximately 8,200 children in the world each year. The average age at diagnosis is between 12 and 18 months. If not detected early, it is the most life-threatening eye cancer in kids.
Researchers say retinoblastoma has a genetic link in 40% of the cases. Patients with retinoblastoma also experience an increased frequency of second malignancies, particularly if the cancer is hereditary. These cancers most often manifest as sarcomas and occur in up to 8% of retinoblastoma patients after 18 years of follow-up.
Interestingly, retinoblastoma can begin to grow before the baby is born. The cancers develop early as the fetus begins to grow. Normally, eye cells develop in an organized manner. But sometimes the cells lining the retina divide and grow out of control, forming retinoblastoma tumors.
If caught early, retinoblastoma is treatable, and the eye can usually be saved. Unfortunately, awareness of this disease is low, and it often goes undiagnosed until the tumors are large, even fill the eye. Failure to catch retinoblastoma early is particularly problematic in developing countries. For instance, in Kenya, 8 out of 10 children diagnosed with this type of eye cancer die from it. In those cases, the tumor continues to grow out of the eye and spreads to other parts of the body.
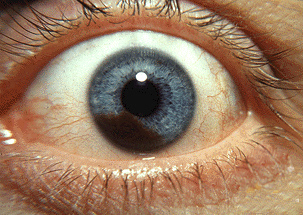
This underscores the importance of routine eye exams for children. Parents should also be aware of signs that could indicate eye cancer. These include a white pupil, unusual squinting, changes in the color of the iris, and painless redness or inflammation of eye. White pupils are sometimes best seen as white reflections showing up in the eye in photos taken with a flash camera. White pupil can indicate the presence of a tumor in the eye.
The Eye Cancer Foundation is working to save children’s lives by improving the diagnosis and treatment of retinoblastoma in developing countries. The Foundation has partnered with the International Council of Ophthalmology (ICO) to promote and conduct eye cancer fellowship education for physicians from under-served countries.
Retinoblastoma doesn’t garner media attention like Leukemia and other more common childhood cancers. But it can be every bit as devastating to the children it affects. Like these other cancers, the key is awareness and early diagnosis.


 The AJCC Cancer Staging Manual defines an international language for oncology. Created with and adopted by the Union for International Cancer Control (UICC), the AJCC-UICC TNM Cancer Classifications enables communication between eye cancer care providers all over the world. The manual brings together all currently available information on staging of cancer, and incorporates newly acquired knowledge on cancer etiology and pathology.
The AJCC Cancer Staging Manual defines an international language for oncology. Created with and adopted by the Union for International Cancer Control (UICC), the AJCC-UICC TNM Cancer Classifications enables communication between eye cancer care providers all over the world. The manual brings together all currently available information on staging of cancer, and incorporates newly acquired knowledge on cancer etiology and pathology.