A study published in August in JAMA Ophthalmology probes the importance of inflammation associated with immune system response in uveal melanoma.
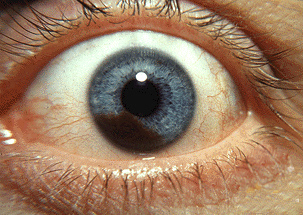
Uveal melanoma is an eye cancer that involves the iris, the muscle surrounding the lens, or the choroid – a vascular layer with connective tissue between the retina and the sclera. It is generally well-controlled by radiation therapy or surgery, but often develops aggressive metastases. Once the cancer spreads to other parts of the body, there are very few cures.
Researchers have found that certain genetic alterations are associated with metastases, but gain in a specific chromosome – 6P – is associated with a more favorable outcome.
Ulrich Pfeffer, PhD with the Laboratory of Molecular Pathology Istituto di Ricovero e Cura a Carattere Scientifico Azienda Ospedaliera Universitaria San Martino in Genoa, Italy, said many have guessed that the immune system, or more generally, inflammation might protect uveal melanomas with this alteration from progression to metastasis.
Seeking to better understand the process, researchers looked at a gene on the 6P chromosome, the putative immunomodulatory BTNL2. An immunomodulator is a chemical agent that modifies the immune response or the functioning of the immune system. Pfeffer described the findings:
“We found highly variable expression of this gene in uveal melanoma samples where it is expressed by tumor cells and by infiltrating immune cells. The type of infiltrate is strongly associated with the risk to develop metastases.”
While the exact operation of BTNL2 and its interaction with the immune system remains unclear, the research does indicate a relationship between immune response and metastasis in uveal melanoma. Pfeffer said this is key:
“Inflammation is an important feature of uveal melanoma and BTNL2 is likely to be an important determinant of the local immunological environment.”
He recommends further research in the hopes effective immunotherapies can be developed:
“BTNL2 is a member of a family of genes that share many features with other immunomodulatory genes. Some of these genes are targets for highly successful therapies. However, many uveal melanoma patients do not respond to these therapies. Future research should address BTNL2 as a specific modulator of the immunological niche of the eye.”
Inflammation is often associated with intraocular melanoma. It can be seen both prior to or after radiation treatment. Signs of inflammation suggest that the patient’s own immune system is trying to reject or destroy the primary cancer.
Another study we reported on last spring found a subset of T-cells in uveal melanoma that had robust anti-tumor reactivity. With further research, it may be possible to build on this knowledge to discover therapies that will boost the immune system’s response and/or effectiveness to successfully treat uveal melanoma.
The studies also underscore the importance of boosting the immune system generally when fighting eye cancer. There are a number of simple steps patients can take to strengthen the immune system, including:
- Eating a healthy, well-balanced diet.
- Getting plenty of sleep.
- Moderate exercise.
- Avoiding excessive stress.
Harvard Health Publications has more detailed information on steps to boost the body’s immune system.









