Chemoreduction of Orbital Tumors
By Paul T. Finger, MD
Note the large nodular basal cell carcinoma on the right lower eye lid and cheek in the image below. It has pulled the eye lid out (cicatricial ectropion) and was found to invade the orbit on CT scan. Click on an image below to enlarge and see the full description:
The diagnosis was easily confirmed by taking a small wedge biopsy in the office. Then after a complete discussion of treatment options, this patient opted for intravenous chemotherapy rather than extensive surgery or radiation therapy. In this case, 3 courses of cis-platinum chemotherapy reduced the size of the tumor. Due to renal toxicity, the treatment was discontinued. Chemoreduction did not (in itself) cure this patient, but it did allow for local resection of the reduced sized-tumor. Under frozen section control, tumor-free margins were obtained.
For more information on the investigational technique we offer the following references.
References
- Luxenberg MN and Guthrie TH, Jr.. Chemotherapy of eyelid and periorbital tumors. Trans Am Ophthal Soc 1985;83:162-180.

After 3 courses of treatment the tumor was noted to shrink and his ectropion diminished. Note the improvement in the CT appearance. - Luxenberg MN and Guthrie TH, Jr.. Chemotherapy of basal cell and squamous cell carcinoma of the eyelids and periorbital tumors. Ophthalmology 1996;93:504-510.
- Morley M, Finger PT, Perlin M, Weiselberg LR, DeBlasio DS. Cis-Platinum Chemotherapy for Ocular Basal Cell Carcinoma. The British Journal of Ophthalmology, 1991, 75, 407-410.
Related Links
Laser Photocoagulation For Radiation Retinopathy
By Paul T. Finger, MD
Dr. Finger uses laser photocoagulation to prevent radiation related retinopathy, maculopathy, and loss of vision. As published in the British Journal of Ophthalmology, Drs. Finger and Kurli found that eyes with posterior choroidal melanomas were more likely to develop sight-threatening radiation retinopathy. In that series, 50 patients were treated with sector scatter laser photocoagulation to clinically evident radiation retinopathy. A second group of patients (considered to be “high risk” to develop radiation retinopathy) were also treated with laser.
In this study, laser photocoagulation improved radiation retinopathy in 29 (64.4%) of the 45 patients treated after the onset of radiation retinopathy (17 with only retinopathy, 10 with a combination of retinopathy and maculopathy, and two with only maculopathy). Of the 16 patients who received laser treatment before clinical evidence of retinopathy, only 1 developed radiation maculopathy and two retinopathy without maculopathy (all three responded to additional laser photocoagulation).
None of the patients in the prophylactic laser group lost more than three lines of vision as a result of maculopathy.
Conclusions
Sector scatter argon laser photocoagulation can be used to induce regression of radiation retinopathy. Though early treatment of radiation retinopathy appears to be more effective, a more long term and prospective randomized study should be performed.
Related Links
18FDG PET/CT SUV: A Noninvasive Biomarker For the Risk of Metastasis from Choroidal Melanoma
By Paul T. Finger, MD
In a research study, Dr. Finger compared the intensity of radioactive glucose uptake [from positron emmission tomography (PET)] to clinical, ultrasound, and pathology features of choroidal melanomas evaluated by FDG positron emission tomography / computed tomography (PET/CT). Ultrasound was used to measure tumor size, evaluate tumor shape and intrinsic vascularity (blood flow). Histopathology and immunohistochemical evaluations of tumor cell-type, necrosis, glycogen-content, vascularity and extrascleral extension were performed.
Selecting out the highest 6 PET/CT standardized uptake values [(SUV) > or = to 4.0] melanomas, patients were (on average) 10 years older. in general, higher SUV tumors had larger basal dimensions, were epithelioid-cell type, were centered anterior to the equator, contained enlarged blood vessels (>150 microns in diameter), and had formed extrascleral extension.
This study suggests that PET/CT imaging offered a physiologic assessment of glucose metabolism within choroidal melanomas. Increased FDG PET/CT SUV ( > or = to 4.0) was positively correlated to known clinical, pathology, and ultrasound features linked to metastatic potential of choroidal melanoma.
Related Links
- View this innovation as it appears in the British Journal of Ophthalmology
- An article that demonstrates how tumor size is correlated to PET/CT SUV
- An article that demonstrates the use of PET/CT for initial screening of patients with choroidal melanoma.
- An article that demonstrates the sites of choroidal melanoma metastasis defined by PET/CT
- Search PubMed for 18FDG PET/CT SUV: A Noninvasive Biomarker For the Risk of Metastasis from Choroidal Melanoma
- Search Google for 18FDG PET/CT SUV: A Noninvasive Biomarker For the Risk of Metastasis from Choroidal Melanoma
25 Gauge Incision Anterior Segment Surgery Found Helpful For Both Tumor Biopsy: The Finger Iridectomy Technique
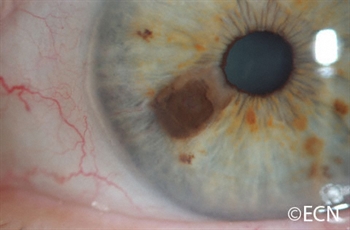
Iris, iridociliary, and other anterior segment tumors can be biopsied to help determine if they are a benign or malignant. In the past, a biopsy was either performed by aspiration through a needle [fine needle aspiration biopsy (FNAB)] or by a surgical iridectomy. The advantage of a needle biopsy was the very small “needle” incision that required no stitches or consequences for vision. Unfortunately, it was difficult to do more that scratch the tumor with the needle while aspirating a few cells. Using a sharp needle, the tumor often bleeds, clouding the view and making biopsy more difficult. In the past, the alternative was a surgical iridectomy that required a relatively large corneal incision, removal of a full-thickness piece of iris and sutures to close the corneal wound.
In an effort to make iris and ciliary body tumor biopsy safer and more effective, Dr. Finger invented a technique for minimally invasive iris biopsy (with less surgical trauma). This new technique combines the benefit of 1-mm typically sutureless incision with the ability to retrieve iris tumor biopsy specimens for pathology analysis. He has used this technique to perform tumor biopsy, iridotomy and to remove iris melanoma.
Dr. Finger has also used this technique to treat narrow angle glaucoma. Dr. Finger says, “it would be particularly useful for the treatment of children and mentally challenged adults who are not able to have the laser iridotomy method.” FIT can be used to surgically create a small hole in the iris through a 25 gauge self-sealing incision. “Micro-incision surgery should be safer for this group of patients who might rub their eye after surgery.”
For more information this technique has been recently published in the British Journal of Ophthalmology and Graefes Archive of Clinical and Experimental Ophthalmology.
The Finger iridectomy technique: small incision biopsy of anterior segment tumors.
Finger PT, Latkany P, Kurli M, Iacob C
The British Journal of Ophthalmology 2005;89:946-949
Small incision surgical iridotomy and iridectomy.
Finger PT.
Graefes Arch Clin Exp Ophthalmol. 2005 Aug 2;:1-2
The Finger Iridectomy Technique for Glaucoma
Finger PT
British Journal of Ophthalmology 2007;91:1089-1090.
Related Links
- Small Incision surgical iridotomy and iridectomy. Graefes Arch Clin Exp Ophthalmol. 2005 Aug 2;:1-2 [Epub ahead of print]
- A New Technique for 25-g Iridotomy, Iridectomy, and Tumor Biopsy – Retinal Physician
- The Finger Iridectomy Technique for Glaucoma – British Journal of Ophthalmology Abstract
- Search PubMed for 25 Gauge Incision Anterior Segment Surgery Found Helpful for Both Tumor Biopsy and Narrow Angle Glaucoma
- Search Google for 25 Gauge Incision Anterior Segment Surgery Found Helpful for Both Tumor Biopsy and Narrow Angle Glaucoma
Amniotic Membrane Is Used To Protect The Cornea During Plaque Radiation Therapy
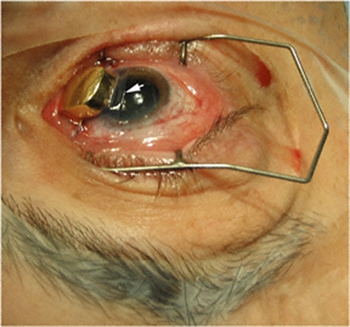
By Paul T. Finger, MD
Patients with melanomas of the iris and ciliary body are more and more commonly treated with plaque radiation therapy. This is because I found radiation to be less invasive and therefore safer than intraocular surgery. Plus, larger areas can be treated with radiation than can be safely removed. This has allowed for excellent local control (tumor destruction) and vision retention. Though many irradiated patients develop radiation cataracts, these can be removed (the same way as other cataracts) restoring excellent vision. At The New York Eye Cancer Center, almost no patients with anterior intraocular melanomas have developed sight-limiting radiation maculopathy or optic neuropathy.
However, in the past, there have been problems associated with placing the radioactive plaque onto the cornea. First, there were concerns about irradiating the cornea. Second, many patients found having a metal device sewn to their cornea for 4-7 days painful.
Dr. Finger has found the cornea tolerated the amount of radiation required to treat iris and ciliary body melanomas. It remained clear for the vast majority of patients. However, having a radiation plaque sewn to the cornea was an uncomfortable procedure.
In an effort to solve this problem, Dr. Finger discovered that a thin, transplanted amniotic membrane tissue could be placed between the gold radiation eye plaque and the cornea during treatment. He simply slides this tissue between the plaque and the cornea during implantation. It is removed 7 days later when the plaque is removed. This technique has made a huge difference – it improved patient comfort and does not affect the radiation treatment.
This note is linked to a You-Tube video demonstrating this new technique. It shows implantation of a plaque onto the cornea and eye wall.
Related Links
- Watch YouTube video of actual “Finger’s Amniotic Membrane Graft Technique” surgery.
- Plaque radiation therapy for malignant melanoma of the iris and ciliary body – American Journal of Ophthalmology
- Tumour location affects the incidence of cataract and retinopathy after ophthalmic plaque radiation therapy – British Journal of Ophthalmology
- Search PubMed for Amniotic Membrane is Used to Protect the Cornea During Plaque Radiation Therapy
- Search Google for Amniotic Membrane is Used to Protect the Cornea During Plaque Radiation Therapy