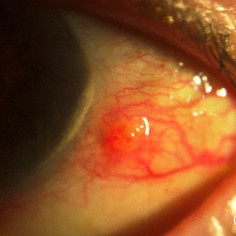
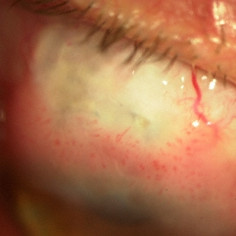
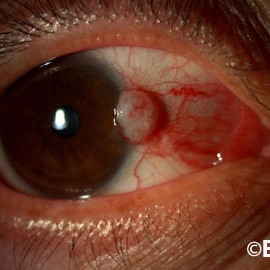
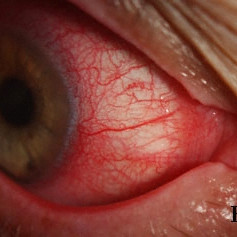
Pyogenic granuloma of the bulbar conjunctiva

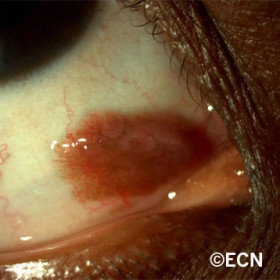
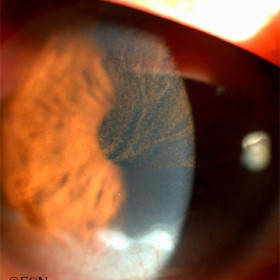
Nevus of the conjunctiva at the plica
Nevus of the conjunctiva at the plica - Slit-lamp photograph demonstrates its cystic components.

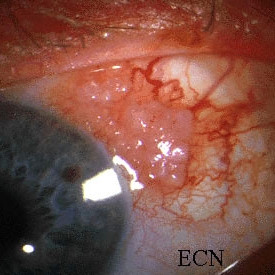
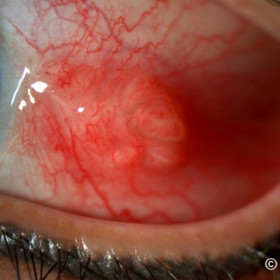
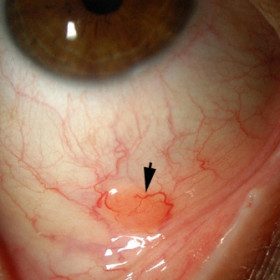
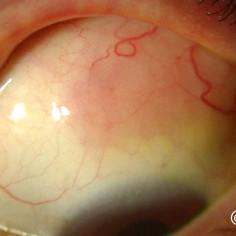
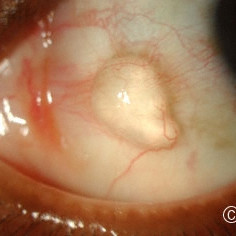
Oncocytoma
Oncocytoma - Red subconjunctival tumor is seen at the plica semilunaris.

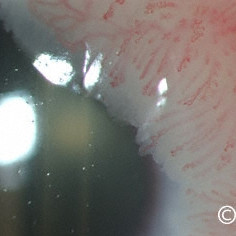
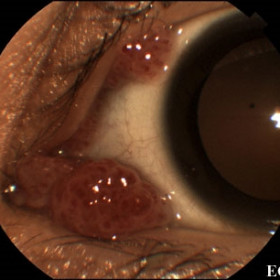
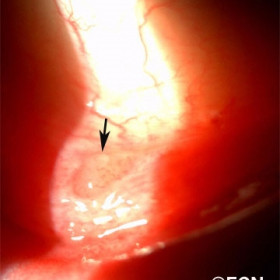
Pedunculated conjunctival papilloma
Pedunculated conjunctival papilloma - Note the fingerlike or cauliflowerlike appearance
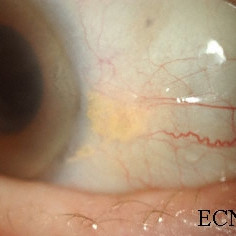
Pingueculum
Pingueculum - Note the bland hypovascular yellow-colored tumor just posterior to the corneal scleral limbus.

Pingueculum
Pingueculum - Slit lamp photography can be used to establish a baseline appearance for future comparison.

Pingueculum - Atypically large
Pingueculum - Atypically large; However it is flat, relatively avascular and without corneal extension.

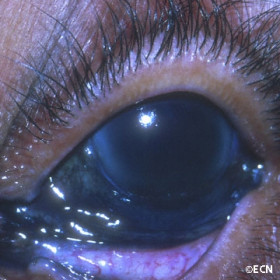
Plical Conjunctival Nevus
Plical Conjunctival Nevus - Slit lamp photograph demonstrates a pigmented plical nevus. Note there are no recruited vessels leading to the nevus.

Post-hemorrhagic chocolate conjunctival cyst

Post-hemorrhagic chocolate cyst
Post-hemorrhagic chocolate cyst after depression with a cotton-tipped applicator

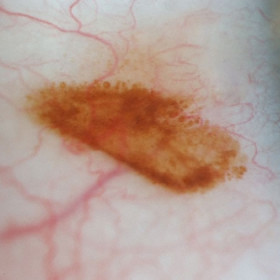
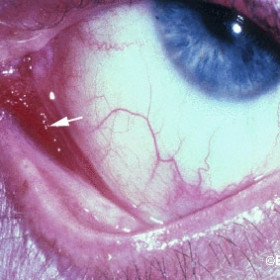
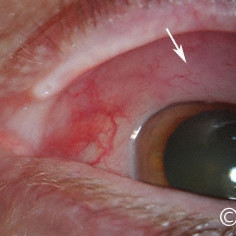
Primary acquired melanosis (PAM)
Primary acquired melanosis (PAM) - A case of new onset unilateral pigmentation (arrow) in a middle aged female.

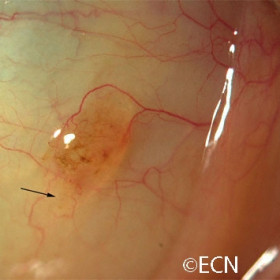
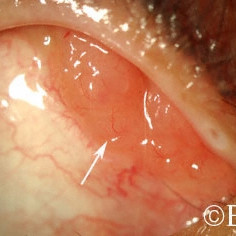
Primary acquired melanosis (PAM)
Primary acquired melanosis (PAM) with pagetoid-like extension onto the corneal epithelium (arrow).

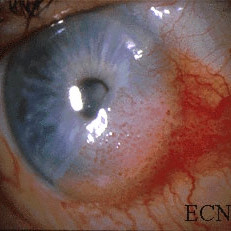
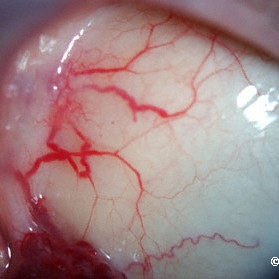
Pterygium
Pterygium - Note the wing shaped fibrovascular growth extending onto the cornea.
Pterygium
Pterygium - This pterygium has grown as to cover part of the pupillary (visual axis) causing loss of vision.

Nevus of Ota
Nevus of Ota - Note the episcleral (ocular melanosis) and eyelid melanosis.
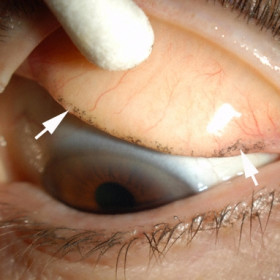
Retained Eyeliner Pigment
Retained Eyeliner Pigment - Note the linear distribution at the superior edge of the tarsus (arrows).
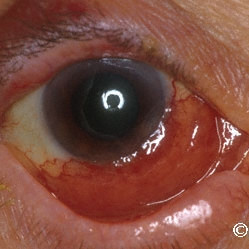
Squamous carcinoma of the conjunctiva
Squamous carcinoma of the conjunctiva - Deep corneal and iris neovascularization (arrows) associated with intraocular invasion.
Squamous carcinoma of the conjunctiva
Squamous carcinoma of the conjunctiva - Squamous conjunctival neoplasia around a filtering bleb for glaucoma
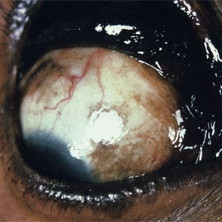
Squamous carcinoma of the conjunctiva
Squamous carcinoma of the conjunctiva - Nodular variant that is more likely to invade the eye.
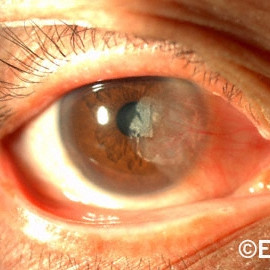
Squamous carcinoma of the conjunctiva and cornea
Squamous carcinoma of the conjunctiva and cornea - Note the corkscrew vessels and a leading edge of gray translucent tumor.
Squamous carcinoma of the conjunctiva with corneal extension
Squamous carcinoma of the conjunctiva with corneal extension - Note the corkscrew shaped blood vessels.

Squamous carcinoma of the conjunctiva with orbital extension.
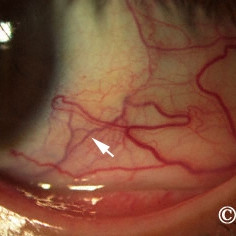
Nodular Squamous Conjunctival Carcinoma
Nodular Squamous Conjunctival Carcinoma - This squamous carcinoma exhibits a few corkscrew vessels on its surface (arrow).
Squamous Conjunctival Papilloma
Squamous Conjunctival Papilloma - Note the atypical hyperpigmentation, fine vasculature and parse tumor stroma.
Squamous papilloma of the conjunctiva.
Squamous papilloma of the conjunctiva. Note the relative thickness of vessels and their surrounding stroma
Suture granuloma
Suture granuloma - subsequently resolved with topical steroid therapy
Topical mitomycin chemotherapy related chemical blepharitis and conjunctivitis

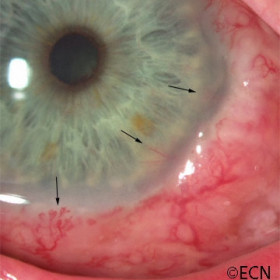
Conjunctival sarcoidosis
Conjunctival sarcoidosis - This case presented with cobblestone granulomas on the bulbar surface (arrows)
Accessory Lacrimal Gland
Accessory Lacrimal Gland- Note that this lesion (arrow) is subconjunctival and located in the fornix.
Atypical Lymphoid Hyperplasia
Atypical Lymphoid Hyperplasia - Slit lamp photograph demonstrates one (arrow) of many conjunctival lymphoid nodules seen in this patient.
Brawny scleritis
Brawny scleritis - Note the deep scleral blood vessels (arrow) beneath the conjunctiva. Scleral thickening and vitreous cells were noted on ultrasound.
Conjunctival Argyrosis
Conjunctival Argyrosis - Conjunctival pigmentation due to drops containing a silver solution
Conjunctival lymphoma
Conjunctival lymphoma - Salmon Patch

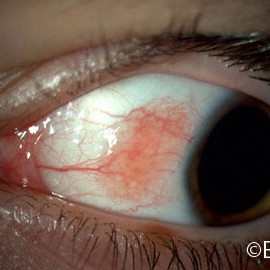
Conjunctival melanoma
Conjunctival melanoma - An episcleral nodule of conjunctival melanoma (arrow).
Conjunctival melanoma
Conjunctival melanoma in a African American patient.
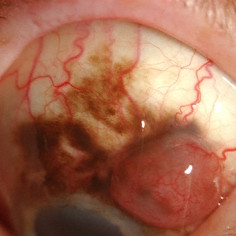
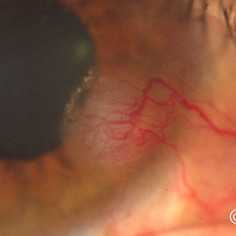
Conjunctival Melanoma with PAM
Conjunctival Nevus
Conjunctival Nevus - Note the multiple rounded cystic components along the edges of the nevus.
Conjunctival Nevus
Conjunctival Nevus - Slit lamp photography documents the margins of this amelanotic conjunctival nevus that does not extend onto the cornea.
Conjunctival nevus
Conjunctival nevus just anterior to the plica

Conjunctival sarciod granuloma
Conjunctival sarciod granuloma in the inferior fornix (arrow).

"Finger-tip" cryotherapy probes
"Finger-tip" cryotherapy probes (enlarged tip inset). Note the spatulated surface.
Corneal melanoma
Corneal melanoma - An amelanotic corneal recurrence of a conjunctival melanoma.
Corneal Melanoma
Corneal Melanoma - Pagetoid corneal extension of a diffuse multifocal conjunctival melanoma.
Epibulbar Conjunctival Cyst
Epibulbar Conjunctival Cyst (see ultrasound images for correlation).

Epibulbar Dermolipoma
Epibulbar Dermolipoma - This epibulbar tumor extends from the cornea to the lacrimal gland.

Iris presenting beneath the conjunctiva
Iris presenting beneath the conjunctiva simulates a malignancy. Not the correctopia, UBM shows no ciliary body neoplasm.
Kaposis sarcoma of the conjunctiva
Kaposis sarcoma of the conjunctiva - Note the fleshy red-colored tumor in the inferonasal fornix (arrow).

Lymphangioma of the conjunctiva
Lymphangioma of the conjunctiva - lymphangiectasia (arrow) associated with an orbital lymphangioma
Lymphangioma of the conjunctiva
Lymphangioma of the conjunctiva - Note the variably sized subconjunctival lymphangiectasias.
Lymphoma of the conjunctiva
Lymphoma of the conjunctiva - The "salmon patch" of malignant conjunctival lymphoma (arrow).
Lymphoma of the conjunctiva
Lymphoma of the conjunctiva - Noted in the supero-nasal fornix (arrow).
Lymphoma of the conjunctiva

Lymphoma of the conjunctiva
Lymphoma of the conjunctiva - Mucosa associated lymphoid tissue (MALT type).