By Paul T. Finger, MD
Description
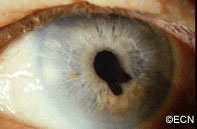
The iris is the colored part of the eye. It is made up of two layers. The outer “stroma” can be blue, hazel, green or brown. The back layer (the iris pigment epithelium) is always brown. Tumors can grow within, through and thus behind the iris.
Symptoms
Iris melanoma patients usually have no symptoms. The tumor might be noticed by the patient, their family, or by the eye care specialist (during a routine eye examination). Some people have lots of freckles on their irides. Some of these pigmented spots have thickness and are called Nevi.
If the patient notices that one of their nevi has changed, enlarged or is pulling (ovalization) on the pupil; they should see an eye care specialist for evaluation and referral to an eye cancer specialist.
Diagnosis
Photographs of the surface of the iris tumor should be obtained to establish a baseline for
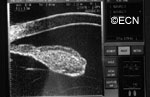
future comparisons. High frequency ultrasound is used to examine and measure the iris tumor. Ultrasound can reveal if the tumor is cystic or solid, how it extends within the iris and ciliary body. Ophthalmic oncologists use high frequency ultrasound measurements to evaluate iris tumors for evidence of growth or regression after treatment.
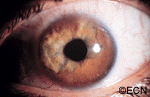
Characteristics that suggest that an iris tumor is cancerous include seeing blood vessels within the tumor (intrinsic vascularity), secondary glaucoma, evidence that the pupil is deformed (ectropion uveae), and the development of a cataract beneath the tumor. Some eyes may have enlarged “sentinel” blood vessels on the white of the eye (sclera) in the quadrant of the tumor.
The most important finding is documented growth. Since iris melanomas are commonly small, and less commonly (10-11%) spread to other parts of the body, these tumors are often watched for evidence of growth or change before biopsy or treatment is considered. A small amount of growth is not thought to significantly affect the rate of metastasis from a small iris melanoma. When necessary, eye cancer specialists can biopsy an iris tumor to help determine if the tumor is benign or malignant.
Treatments
Most pigmented iris tumors do not grow. They are photographed and monitored with periodic observation. When an iris melanoma is documented to grow, we know that it can damage the eye, cause secondary glaucoma and spread to other parts of the body. Then treatment risks become more acceptable to the patient. At The New York Eye Cancer Center, we typically use plaque radiation to destroy iris and iridociliary melanomas. This treatment allows for preservation of the iris, the pupil and does not cloud the cornea. We have found that the most common complication is cataract and permanent vision loss is rare.
Small Iris Melanomas:
Though most small iris melanomas can be surgically removed, however iridectomy may cause glare and astigmatism. The function of the iris and size of the pupil are better preserved if the tumor is destroyed with plaque radiation.
Medium-sized Iris Melanomas:
Though many of these tumors can be surgically removed, plaque or proton radiotherapy should be considered as primary treatment for these tumors. Though a radiation cataract is likely to develop, due to the distance between the radiation and the macular retina, vision limiting radiation retinopathy is very unlikely.
Large-sized Iris Melanomas with Advanced Glaucoma:
These cases can often be difficult to treat with either surgical removal or eye-sparing radiation therapy. Cure for these tumors is likely to require removal of the eye.
Diffuse Iris Melanomas:
Sometimes the entire iris is filled with melanoma. In these cases, removal of the eye is a reasonable option. However, there has been a recent trend towards and our experience that eye and vision-sparing radiation of the entire front of the eye (anterior segment) can be used to control the tumor, spare vision and allow the patient to keep their eye.
Related links
- Read About Radiation for Iris and Ciliary Body Melanoma
- Read the Scientific Literature about Iris Melanoma
- Read About Dr. Finger’s Small Incision Iris Biopsy Technique (or Finger Iridectomy Technique)
- Search PubMed for Iris Melanoma
- Search the Internet about Iris Melanoma
- Read About a Multicenter International Study fo Iris Melanomas









