The Nevus of Ota
By Paul T. Finger, MD
Description

Patients with the Nevus of Ota have increased amounts of melanin (pigment) and melanin producing cells (melanocytes) in and around their eyes. This includes the intraocular blood vessel layer called the uvea (choroid, ciliary body, and iris), on the white part of the eye ball (sclera), and in the eyelids.
Patients with the Nevus of Ota have been shown to be at greater risk for the development of intraocular and central nervous system malignant melanomas (e.g. choroidal melanoma). Though intraocular melanomas are more common in these patients, their lifetime risk is though to be 4%.
Patients with the Nevus of Ota should be examined at least every 6 months by an eye-cancer specialist and a neurologist.
Symptoms
The Nevus of Ota appears as increased pigmentation of one eye and its eyelids. The eyelid is darkened, pigment can be observed on the white of the eye and that iris may be darker (compared to the contralateral iris). Though none of these findings produces physical symptoms, physical asymmetry can have a psychological impact on the patient.
Ocular Melanosis is diagnosed in cases of ocular melanosis there is no eyelid involvement.
Diagnosis
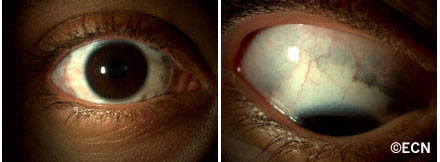
Careful inspection of any patient with two different colored irises (heterochromia irides) may uncover the eyelid and episcleral pigmentation diagnostic of the Nevus of Ota.
Slit-lamp biomicroscopy is used to distinguish between conjunctival and episcleral pigmentation. Comparative examination of the irides can be used to evaluate coloration and surface characteristics.
Dilated ophthalmoscopy similarly demonstrates asymmetric “darker” pigmentation of the choroidal vascular layer beneath one retina.
Ophthalmic ultrasound imaging will reveal thickening of the vascular uveal layer of the eye. Examinations should include both posterior and anterior segment (UBM) imaging.
Treatments
Most patients with the Nevus of Ota have no subsequent related problems.
Less than 4% can develop choroidal melanoma in the affected eye. Fewer will develop intracranial neoplasia. Therefore, it is reasonable for all patients with the Nevus of Ota to have twice yearly eye examinations with dilated ophthalmoscopy. They should also have an initial neurology assessment, followed by periodic medical evaluations.









