Owing to the lack of a prognosis related classification for radiation retinopathy, and the need for a common language for comparative studies, this study prompted the creation of the classification presented in the table below. There are certain preproliferative findings associated with radiation treatment of the eye.
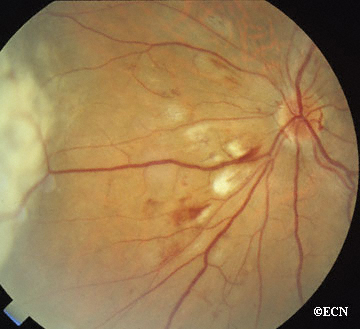
Ophthalmoscopy is best used to view such common findings as cotton wool spots, retinal haemorrhages, ghost vessels, exudates and the less frequent retinal microaneurysms and uveal effusions. Fluorescein and indocyaninegreen angiography are typically used to define the extent of retinal ischaemia and vascular anomalies (table 5).
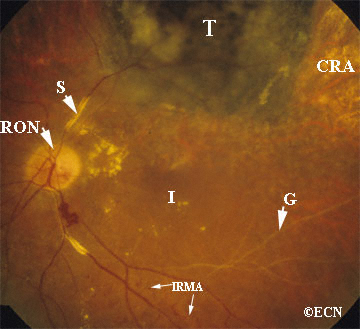
When located outside the macula, stage 1 findings are consistent with excellent central vision and a good visual prognosis (mild risk). In contrast, stage 2 radiation retinopathy requires that these pathological findings are located in the macula and therefore carry a more guarded prognosis for vision (moderate risk). When the eye enters stage 3, some vision loss has probably occurred and the prognosis for return to pretreatment vision is poor (severe risk). Despite its location, the presence of retinal neovascularisation is ominous. It suggests a profound ischaemic drive and carries a worse prognosis for long term visual acuity (table 5). Vitreous haemorrhage, large areas of retinal ischaemia, and iris neovascularisation are associated with a worse prognosis for vision and globe salvage (table 5). Vitreous haemorrhage clouds our ability to use laser treatment and to monitor the progression of radiation retinopathy. Patients who present with vitreous haemorrhage often have occult neovascularisation and are at risk for ghost cell or neovascular glaucoma.
The Finger Classification of Radiation Retinopathy
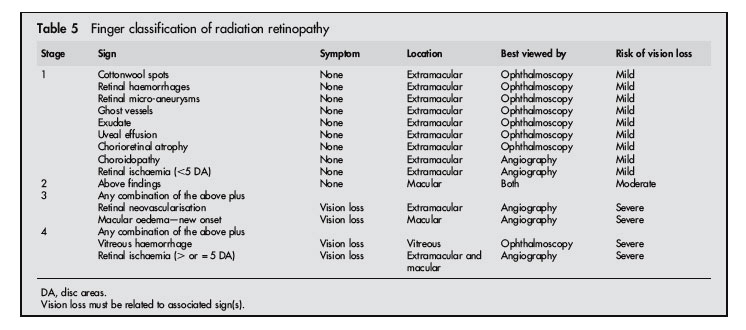
Table from Finger and Kurli, Br J Ophthalmol 2005;89:730–738. doi: 10.1136/bjo.2004.052159









