Brachytherapy Boost For Orbital Tumors
By Paul T. Finger, MD
Dr. Finger has been using the Brachytherapy Boost Technique (BBT) for over 25 years. It is a multidisciplinary approach that can spare patients from exenteration surgery (removal of the eye and all the orbital contents).
During the BBT procedure, instead of removing the eye lids and orbital tissues, the bulk of the orbital tumor is removed and radioactive seeds or HDR catheters are temporarily placed in the tumor-bed. With this method, the area of tumor infiltration is irradiated more than the rest of the remaining ocular and/or orbital structures. An overlay of a reduced amount of external beam radiation therapy is typically given to the entire orbit or targeted zone.
Dr. Finger considers the brachytherapy boost technique in the following clinical situations
1. When the standard external beam radiotherapy would require using a dose so high that it would result in a blind and painful eye (e.g. orbital melanoma, squamous and basal cell carcinoma, adenoid cystic carcinoma).

2. When exenteration of the orbit is the only option, but offers historically poor local control rates (e.g. adenoid cystic carcinoma).
3. When a patient refuses exenteration surgery.
Related Links
- Search PubMed for Brachytherapy Boost For Orbital Tumors
- Search Google for Brachytherapy Boost For Orbital Tumors

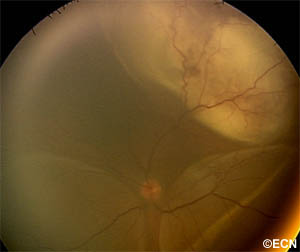

![[10 MHz] 3D Ultrasonography Reveals - *Note* Ultrasonography reveals an open funnel retinal detachment (white arrow). Note the echolucent vitreous humor. The posterior choroidal detachments (black arrows) exhibit variable internal reflectivity consistent with blood. A = anterior, S = superior, T = temporal.](https://eyecancer.com/wp-content/uploads/2016/05/case111.gif)








