Chemoreduction of Orbital Tumors
By Paul T. Finger, MD
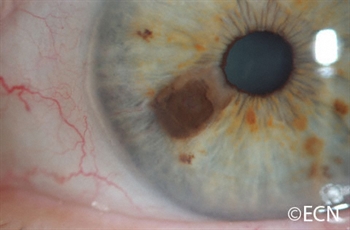
Note the large nodular basal cell carcinoma on the right lower eye lid and cheek in the image below. It has pulled the eye lid out (cicatricial ectropion) and was found to invade the orbit on CT scan. Click on an image below to enlarge and see the full description:
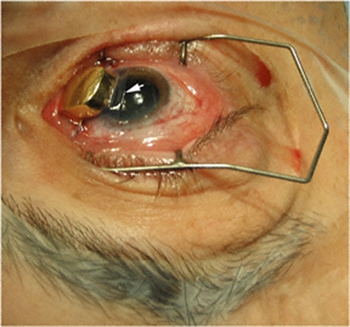
The diagnosis was easily confirmed by taking a small wedge biopsy in the office. Then after a complete discussion of treatment options, this patient opted for intravenous chemotherapy rather than extensive surgery or radiation therapy. In this case, 3 courses of cis-platinum chemotherapy reduced the size of the tumor. Due to renal toxicity, the treatment was discontinued. Chemoreduction did not (in itself) cure this patient, but it did allow for local resection of the reduced sized-tumor. Under frozen section control, tumor-free margins were obtained.
For more information on the investigational technique we offer the following references.
References
- Luxenberg MN and Guthrie TH, Jr.. Chemotherapy of eyelid and periorbital tumors. Trans Am Ophthal Soc 1985;83:162-180.
After 3 courses of treatment the tumor was noted to shrink and his ectropion diminished. Note the improvement in the CT appearance. - Luxenberg MN and Guthrie TH, Jr.. Chemotherapy of basal cell and squamous cell carcinoma of the eyelids and periorbital tumors. Ophthalmology 1996;93:504-510.
- Morley M, Finger PT, Perlin M, Weiselberg LR, DeBlasio DS. Cis-Platinum Chemotherapy for Ocular Basal Cell Carcinoma. The British Journal of Ophthalmology, 1991, 75, 407-410.