NYECC’s Research Reaches Patients In Russia
Прочитайте эту статью на русском языке
Dr. Finger recently published a scholarly article in the Russian Ophthalmological Journal. The paper chronicles the successful diagnosis and treatment of a 9-month-old girl.
The case was particularly significant because Dr. Finger was able to diagnose and cure the girl through essentially non-invasive treatments. The diagnosis was made clinically without a biopsy and treatment was accomplished solely through the use of steroids.
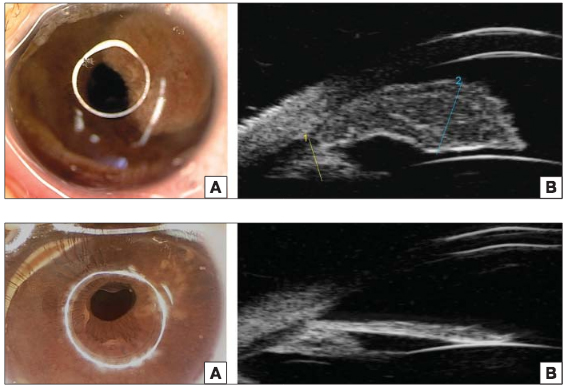
The infant was sent to Dr. Finger for evaluation of a spot on her iris. Slit-lamp examination revealed a left iris tumor that obscured the iris from pupillary margin to ciliary body, as you can see in the top two panels of the image below. Further examination via ultrasound biomicroscopy (UBM) led to a diagnosis of juvenile xanthogranuloma, which is a benign histiocytic skin disorder that primarily affects infants and children.
Dr. Finger treated the tumor with an injection of 20 mg of long acting sub Tenon’s corticosteroid followed by administration of topical steroid ointment four times per day. Within two weeks of the injection, the tumor had diminished to a flat whitish scar. Four and a half months after treatment began, there was no residual tumor visible, as shown in the bottom panels of this photo:
By publishing the results in the Russian Ophthalmological Journal, Dr. Finger’s successful treatment can be replicated to help patients across the Russophone world.
Few clinics engage in this level of international collaboration. Dr. Finger and his colleagues at NYECC are passionate about improving eye cancer diagnosis and treatment not just in North America, but around the world.
“Исследования Нью-Йорского Центра Онкологии Глаза Достигли Пациентов в России.
Доктор Фингер недавно опубликовал научную статью в Российском Офтальмологическом Журнале. Статья приводит описание клинического случая успешного диагноза и лечения 9-месячной девочки.
Этот клинический случай был уникален тем, что Доктор Фингер смог поставить диагноз и вылечить пациентку практически неинвазивным способом: без биопсии, и при применении кортикостероидов.
Новорожденная девочка была направлена к Доктору Фингер на осмотр пятна на радужной оболочке глаза. Осмотр выявил опухоль, распространившуюся от края зрачка до цилиарного тела, как видно на верхней половине снимка. Осмотр ультразвуковым биомикроскопом привел к диагнозу ювенильной ксантогранулемы. Это доброкачественная опухоль кожи, встречающаяся в основном у детей раннего возраста.
Доктор Фингер вылечил опухоль при помощи 20 миллиграмм локальной субэписклеральной инъекции кортикостероида и стероидной мази, применяемой четыре раза в день. В течении последующих двух недель, опухоль превратилась плоский белесый шрам. Четыре с половиной месяца после начала лечения опухоли не стало видно, как продемонстрировано на нижней половине снимка.
Публикация результатов этого успешного лечения, проведенного Доктором Фингер, в Российском Офтальмологическом Журнале позволяет так же успешно вылечить подобных пациентов в русско-язычных странах.
Немногие клиники в мире могут продемонстрировать такой уровень международного сотрудничества. Доктор Фингер и его коллеги в Нью-Йорском Центре Онкологии Глаза всегда стремятся улучшить диагностику и лечение опухолевых заболеваний глаза не только в Северной Америке, но и во всем мире.”




 Dr. Paul Finger of the New York Eye Cancer Center is honored to be the sole author of all eye cancer sections in the latest edition of the Manual of Clinical Oncology. Published last September, the Manual is an essential reference text for clinicians treating and caring for oncology patients anywhere on the globe.
Dr. Paul Finger of the New York Eye Cancer Center is honored to be the sole author of all eye cancer sections in the latest edition of the Manual of Clinical Oncology. Published last September, the Manual is an essential reference text for clinicians treating and caring for oncology patients anywhere on the globe. Dr. Paul Finger has been named one of the
Dr. Paul Finger has been named one of the 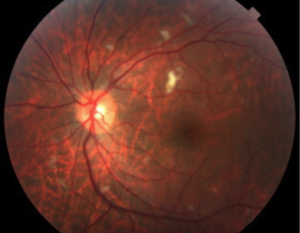 Through his extensive research, Dr. Finger has shown that not all radiation techniques for treating eye cancer are equal.
Through his extensive research, Dr. Finger has shown that not all radiation techniques for treating eye cancer are equal. Although ocular melanoma can spread to other parts of the body, it is important to know that most patients do not develop metastases. However, because there is a risk, we highly recommend initial and follow up systemic evaluations.
Although ocular melanoma can spread to other parts of the body, it is important to know that most patients do not develop metastases. However, because there is a risk, we highly recommend initial and follow up systemic evaluations.







