Ophthalmic Ultrasound Imaging
Dr. Finger recommends the use of high-resolution 20-50 MHz B-scan in movie-mode to measure most intraocular tumors. At the time of diagnosis, he personally performs or reviews each patient’s ultrasound images to ensure all measurements are excellent. During surgery, Dr. Finger performs intraoperative ultrasound imaging to check radiation plaque placement. He broke new ground with the use of new diagnostic imaging techniques, including high frequency and 3D ultrasound for imaging tumors on and in the front of the eye.
Specifically, Dr. Finger and his associates first described the use of 3D ultrasound for measurement of choroidal melanomas, to document proper radioactive plaque placement, and for extrascleral tumor extension.
Dr. Finger and his colleagues have pioneered the use of computerized coronal C-scan ultrasound sections to measure the orbital portion of the optic nerve, to detect optic nerve sheath meningiomas and invasion of retinoblastoma into the optic nerve.
Dr. Finger and coworkers have helped establish the use of high-frequency ultrasound (UBM) imaging for anterior segment tumors (melanocytoma, melanoma, cysts). He has written on the use of high-frequency ultrasound for the diagnosis of conjunctival squamous carcinoma, periocular oncocytoma, Rosai Dorfman Disease, ciliary body adenocarcinoma) and eyelid tumors. He has shown how high frequency ultrasound can be used to detect retinoblastoma that are hidden behind the iris, invasion of conjunctival tumors into the eye, for measurement of iris and ciliary body tumors and to allow for plaque radiation therapy. Ultrasound movies allow him to replay and show patients their tumors and how he measures them.
High-Definition (HD) Digital Photography
Dr. Finger uses the newest technology for imaging, documenting and comparing eye tumors to monitor for growth. Angiograms are used to determine patterns of tumor circulation and response to treatment. Imaging of the eye requires specialized, HD ophthalmic, high-definition digital cameras. Each examination room is equipped with the latest 55″ ultra high-resolution 4K flat screens. Dr. Finger knows there is no substitute for side-by-side comparative photography to detect small changes on or around tumors of the eye. In addition, Dr. Finger has shown that early detection and treatment of radiation eye damage offers the best chance to maintain vision and use of the eye.
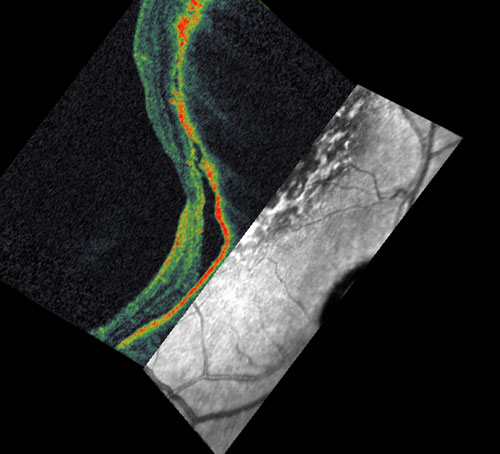
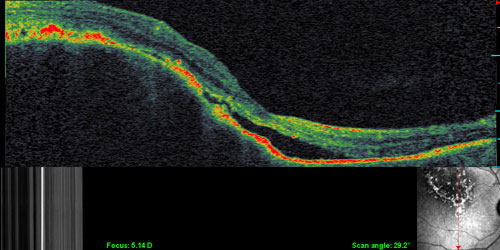
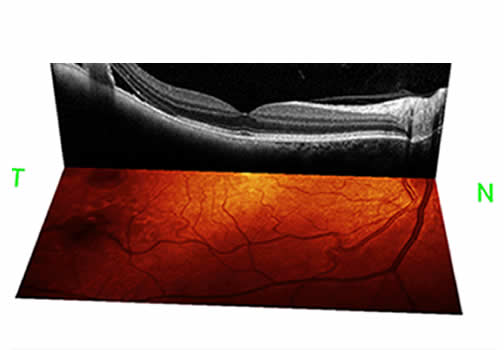
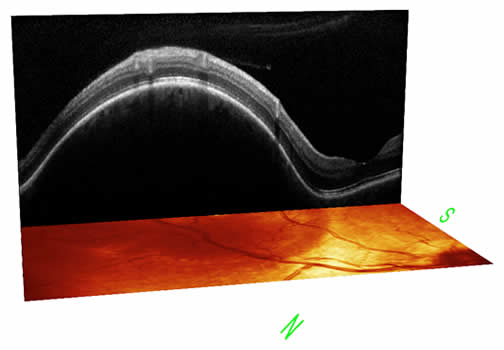
OCT Imaging
Dr. Finger uses a state-of-the-art OCT2 (optical coherence tomography) imaging system. The OCT technique creates 3D images of the retina and is one of the best tools available for the diagnosis of eye cancer.
In December 2015, NYECC became the first clinic in the United States to use the state-of-art OCT2 imaging machine in a clinical setting. The OCT2 represents a huge step forward in imaging technology. Using the OCT2, Dr. Finger can see within, around, and even behind intraocular tumors. With this imaging technology, he can diagnose intraocular tumors, monitor tumor response to treatment, and modulate new vision-sparing ant-VEGF treatments (for radiation retinopathy and optic neuropathy).
The OCT2 features significant advances over the older technology:
- 3D visualizations
- High-resolution images
- Ultra-high density scans
- Full Depth Imaging
- Faster scanning speed for patient convenience
- Records high-speed angiography to visualize blood flow within the eye for better diagnosis
- Upgradable as technology emerges

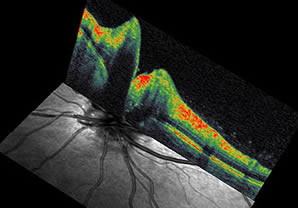
Below are photos taken with OCT for patients with choroidal melanoma (Patient 1 and 2), choroidal hemangioma (Patient 3).
(click on the images below to enlarge)
Total Body FDG PET/CT Imaging
Dr. Finger has pioneered the use of total body 18 FDG PET/CT imaging for choroidal melanoma and other eye cancers. This is because he recognized that the old methods of metastatic screening were often inadequate.
Positron emission tomography allowed for a metabolic assessment of intraocular and orbital tumor metabolism, while computed tomography (CT) allowed us to measure tumor size, shape and relationship to normal anatomic structures. . By overlapping the metabolic and anatomic images, for the first time, PET/CT put form and function on the same diagnostic page.
Dr. Finger’s group also found that intraocular melanomas had different metabolic intensities, further that metastatic melanoma was found at greater frequency outside the liver (primarily bone and skin) than previously thought. However, he still notes that even with FDG PET/CT, microscopic metastasis may not be found.
In his studies, Dr. Finger noted that since bone was the second most common site of metastasis and only a total body scan can detect bone metastasis, “any other tests may come up short.”
Since that time, Dr. Finger and co-workers have used this technique to diagnose patients with metastatic cancers to the eye as well as ocular sebaceous carcinoma, conjunctival melanoma and orbital lymphoma.
Dr. Finger has performed a research study comparing the metabolism of choroidal melanomas as measured by PET/CT against known epidemiologic, anatomic, ultrasonographic and histopathologic risk factors for the development of metastatic choroidal melanoma. This study suggests that a tumor’s metabolic rate can be used to help indicate the risk of metastasis.