Day 4: Live From the ISOO 2019!
Day 4 at the ISOO: Retinoblastoma
Every two years, eye cancer specialists worldwide convene at the International Society of Ocular Oncology Conference in order to review latest research and encourage international collaboration within the field of ophthalmic oncology.
For details on the ISOO Biennial Conference, read more here.
Preventing Retinoblastoma
Dr. Helen Dimaras opened with her talk on clinically preventable retinoblastoma, having analyzed the frequency of unfavorable outcomes such as death, metastasis, enucleation, EBRT, and how we can avoid such outcomes. Looking at data retrospectively allows physicians to “review how patients do and improve practice by looking at the past, reducing errors, and improving documentation and precision of care.”
In high-income nations, frequency of poor outcomes is low, and we need to work on expanding such rates abroad. Not only this, but a comment from the audience emphasized the significance of this study’s call to action: even just one child who succumbs to retinoblastoma is a child lost, and such outcomes need to be taken very seriously. We need to avoid misdiagnosis and under-treatment as much we humanly can to ensure that unfavorable outcomes do not happen in the future.
“Chemoplaques”
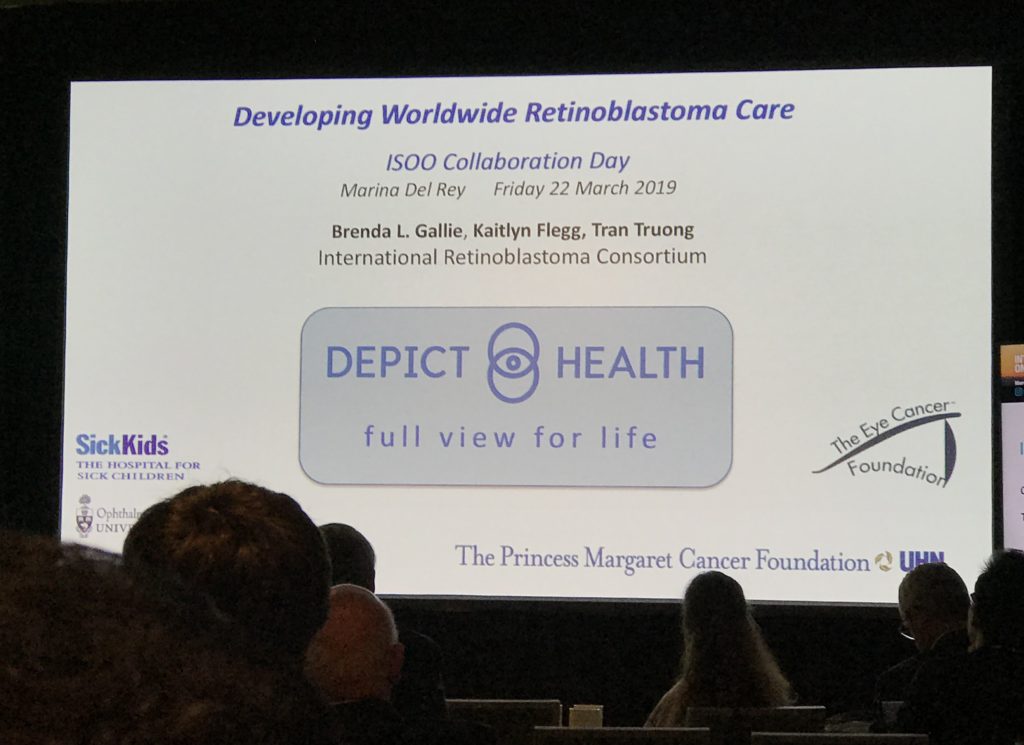
Dr. Brenda Gallie presented an interesting study regarding a device named “chemoplaques” in Chemoplaque (sustained-release topotecan episcleral device) for retinoblastoma: Opportunity for rapid clinical evaluation of toxicity and efficacy to support safe eye salvage. The devise works through continuous exposure via diffusion, and has thus far produced promising results. By day 28, most of the studied tumors had gone away, and many were gone even earlier, by day 18.
International Fellowship Training Guidelines

In an auxiliary lecture hall, many of us gathered to discuss training fellows all over the world in order to create and develop international treatment centers that will allow greater access to eye cancer care in underdeveloped countries and underserved areas. Sound familiar? As this is one of the primary missions of The Eye Cancer Foundation, Chairman of the ECF, Dr. Finger gave a lecture and lead the discussion.

So what is the plan of action? Flexible fellowships with candidates sent from the ophthalmic society of the unserved or underserved region. Being underserved locations, we must be open to 3-month long fellowships, since the physician is needed in their country to give care. 12-month fellowships oftentimes are unfeasible. We must also make a collaborative effort to increase funding for such programs. Dr. Finger says “It has been my experience that funding can come from unexpected places. All you need to do is discuss this wonderful work we are doing and relate how we need help. It is a blessing to allow others to share in the accomplishment of saving children’s sight and life.”
Full video of Dr. Finger’s Lecture Here!