Iris Biopsy 101: The Finger Iridectomy Technique
In order to examine the existence and extent of an iris tumor, a biopsy may be required — but what is a biopsy, exactly? For those who may be unfamiliar with the term, a biopsy is a sampling of tissue taken from a certain area of the body in order for doctors to closely evaluate a patient’s pathology. Every biopsy is different. However, they can sometimes be invasive and cause discomfort. For a patient undergoing a biopsy in an area as delicate as the eye, this may feel intimidating.
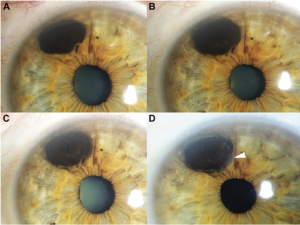
This important factor has contributed to Dr. Finger’s development of the Finger Iridectomy Technique (F.I.T), a minimally invasive but very effective method of biopsy. This technique allows for a large amount of tissues and cells to be biopsied, optimizing sample size while minimizing discomfort for patients.
In this video, Dr. Krystine Olszewski from the New York Eye Cancer Center provides an approachable checklist on what to do before and after an iris biopsy. She discusses the required medication to be taken, as well as what is to be expected in the follow up exam.
Iris Biopsy; Finger Iridectomy Technique from Paul T Finger on Vimeo.
To stay tuned for upcoming videos as well as be informed on all the latest updates in eye cancer research, keep Eyecancer.com, the website for the New York Eye Cancer Center, in your bookmarks!