7 Questions You Should Ask Your Doctor
1. Does your doctor spend as much time as you need to understand your condition and treatment options?
We all know the trend of medicine over the past several decades: doctors’ decisions are being pressured by outside forces and patients feel like they are being rushed along a conveyor belt of care.
At The New York Eye Cancer Center, Dr. Finger and his staff take the time to understand each patient’s needs, answer all questions, and ensure that critical details do not go overlooked.
This is why our practice does not directly participate in many major insurance plans – though we will assist patients seeking reimbursement. Our first priority is patient care that will not be sacrificed to government, hospital, or insurance company demands.
2. Which doctor will perform your surgery?
When you are referred to a specific doctor, you should see that doctor for the initial consultation and in the operating room. You should know what role other doctors, associates, fellows, or residents are taking in your procedures.
At The New York Eye Cancer Center, we think patients deserve to know who will be the primary surgeon for their operations. Your consultation and surgery will be performed by Dr. Finger, who has over 30 years experience treating eye cancers.
3. Who answers the office phone at night?
Find out who answers the phone after hours. Is it a voicemail or will you be sent to the emergency room after office hours?
At The New York Eye Cancer Center, our staff of doctors are trained to answer questions during the day, but care extends beyond office hours. We always have a live person answering our phone even after the office is closed. This ensures that emergencies will be handled by Dr. Finger or his staff at all times. In addition, non-emergency messages will be delivered to The New York Eye Cancer Center office every morning.
4. How familiar is your doctor with established and new treatments? What innovative treatments has your doctor developed?
Look up your doctor before you have your consultation. You can search their publications on http://pubmed.gov. You can also visit the doctor’s web site to evaluate their training.
Dr. Finger has written review articles on eye surgery, radiation, chemotherapy, and metastasis. He recently published the chapter on intraocular melanoma for DeVita’s Textbook of Medical Oncology, as well as the chapter covering all eye cancers in the UICC Manual of Clinical Ophthalmic Oncology.
Patients should also consider seeking a physician who actively contributes to medical advancements. This is not simply for the benefit of mankind, but demonstrates the doctor’s knowledge about his specialty’s state of the art.
Dr. Finger is a pioneer in his field, with 14 filed patents/trademarks and over 300 published medical journal articles and book chapters. Dr. Finger has developed many new medical devices, as well as innovative diagnostic and surgical techniques.
5. Does your doctor publish their results?
Clearly, patients do not want the most popular or the most sociable doctor – they want the doctor who will deliver the highest possible chance of preserving their life and their sight.
At The New York Eye Cancer Center, we have a long history of publishing our results in the medical literature. Recently, we were the first to place summaries of our published results online so that prospective patients can easily access them.
6. Will you be trapped in a system?
Many centers and insurance companies are run as self-contained medical systems. That means every aspect of your care is given within that system (consultations, surgery, radiation, chemotherapy, surveillance). While one-stop-shopping may be easy, it also can prevent you from seeing excellent physicians outside that network.
Dr. Finger is in private practice, so he is able to work with a network of independent service providers that stretch across New York City. Dr. Finger has the freedom to choose his preferred providers for each individual service. The result is his “dream team” of professionals who are each at the top of their field.
7. Are you treated with respect by all practice staff?
Cancer patients know the importance of hope and positivity in surviving this disease. Though appointments may unavoidably cause some anxiety, the doctor’s office should be a place to reinvigorate you in your battle. Patients deserve to be treated with care and respect not just by the doctor, but also by the front desk, billing, optometry, and other office staff. Patients should not be left waiting all day for a scheduled appointment. When emergencies are fit into the schedule, the staff should tell you and make you as comfortable as possible.
The New York Eye Cancer Center prides itself on the quality of each member of its staff. Every patient receives the highest level of care and respect, as you deserve.

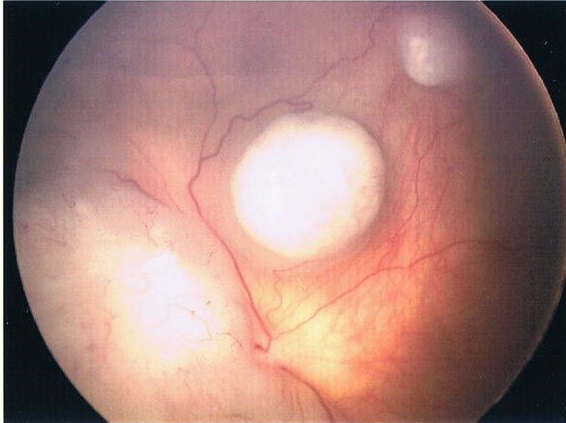

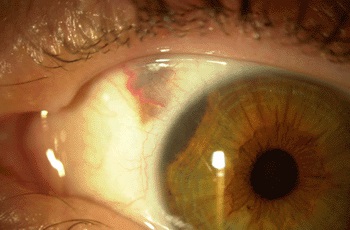
 who were diagnosed at different stages in the disease. This allowed him to observe a wide variety of treatment regimens, including systemic chemotherapy, intraocular chemotherapy, intra-arterial systemic chemotherapy, focal consolidation therapies (e.g. laser and “freezing” cryotherapy), radioactive plaque therapy, external beam radiation therapy, and when necessary – removal of cancer-filled eyes.
who were diagnosed at different stages in the disease. This allowed him to observe a wide variety of treatment regimens, including systemic chemotherapy, intraocular chemotherapy, intra-arterial systemic chemotherapy, focal consolidation therapies (e.g. laser and “freezing” cryotherapy), radioactive plaque therapy, external beam radiation therapy, and when necessary – removal of cancer-filled eyes.