Patients diagnosed with choroidal melanoma run the risk of having the cancer spread to other parts of their body. In fact, medical evidence suggests half of all choroidal melanoma patients will develop metastatic disease. However, Dr. Paul Finger’s says, “It’s not that simple.”
Studies have pinpointed a number of factors shown to affect the spread of ocular melanoma. For example, the Collaborative Ocular Melanoma Study found that younger patients are less likely to develop systemic spread. The Ophthalmic Oncology Task Force found that patients whose intraocular tumors recur after treatment are at higher risk for metastasis. Most significantly, evidence confirmed by The American Joint Committee on Cancer clearly shows that the larger the choroidal melanoma, the higher the risk for metastasis.
This is why early detection and prompt effective treatment of choroidal melanoma saves lives. Without a curative treatment for metastatic disease, Dr. Finger says “destruction of the eye tumor offers the patient his or her best chance for survival.”
Malignant choroidal melanoma develops in the blood-vessel layer “choroid” beneath the retina. About six out of one million people in North America will be diagnosed with a choroidal melanoma each year.
Dr. Finger treats ocular melanoma patients every day. He wrote the chapters on choroidal melanoma in DeVita’s Medical Oncology Textbook, along with The International Union for Cancer Control’s Manual of Clinical Oncology. Through his review of the world’s literature, the accumulation of 31 years experience treating patients, and by performing innovative clinical research, Dr. Finger has confirmed several factors that indicate an increased risk for metastasis. These include tumor size, the age of the patient, and how quickly the tumor is destroyed or removed.
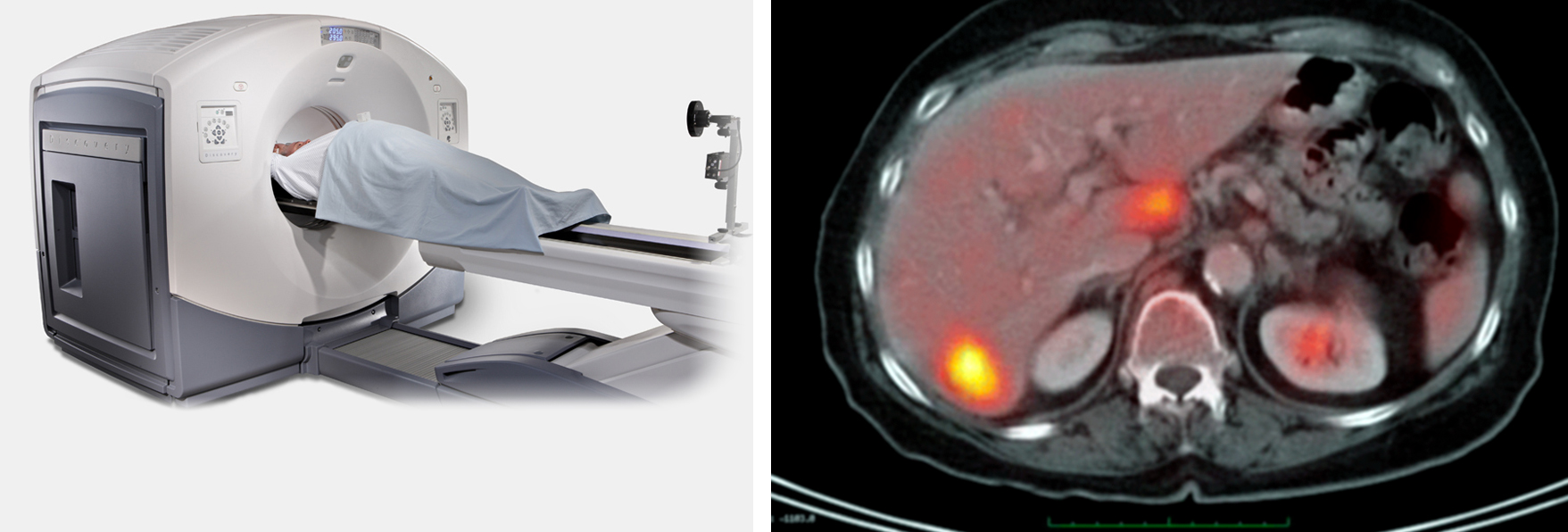
Based on these risk factors and the diagnosis, Dr. Finger determines how to approach metastatic screening for each of his patients. Once the plan is in place, he has the best tools in the world at his disposal. First investigated at the New York Eye Cancer Center, PET/CT screening is the only method that surveys the entire body for metastatic spread. In addition to an initial PET/CT scan, Dr. Finger utilizes subsequent MRI, CT, and ultrasound screening.
Monitoring for cancer spread in choroidal melanoma patients is not a one-size-fits-all process. Dr. Finger approaches it on a patient-by-patient basis, taking into consideration all of the relevant factors.
For more information on metastatic melanoma workup, Download the PDF Here.









