Choroidal Melanoma
 Malignant “choroidal” melanoma arise from the blood-vessel layer “choroid” beneath the retina. In North America, 6 out of each million people will be diagnosed with a choroidal melanoma each year. Malignant choroidal melanomas can spread to other parts of the body.
Malignant “choroidal” melanoma arise from the blood-vessel layer “choroid” beneath the retina. In North America, 6 out of each million people will be diagnosed with a choroidal melanoma each year. Malignant choroidal melanomas can spread to other parts of the body.
Eye cancer specialists determine if you have a choroidal melanoma by performing a complete eye examination. This includes asking questions about your medical history, examining both of your eyes, looking into the eye through a dilated pupil at the tumor, performing an ultrasound examination, and specialized photography. The latter will likely include angiography, optical coherence tomography (OCT and OCT-A) and fundus auto-fluorescence (FAF). For anterior tumors we made need slit-lamp photography, gonio-photography, iris angiography and high-frequency ultrasound imaging (UBM).
Your specialist will also request that you have a complete general medical check up and specific tests depending upon what they see inside your eye. Using clinical testing in the office, the eye cancer specialist should be able to correctly diagnose an intraocular choroidal melanoma in over 96% of cases (without a biopsy). Diagnostic biopsies are typically needed for atypical tumors.
Symptoms
 |
 |
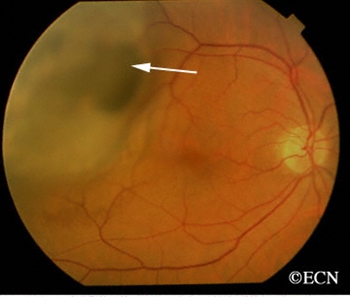
| A dynamic 10 MHz ultrasound reveals the “twinkling” of blood as it flows within a choroidal melanoma. | Choroidal melanoma with orange pigment (arrows). |
Most choroidal melanoma patients have no symptoms and the melanoma is found on routine eye examination. If patients have choroidal melanoma symptoms, they are usually seeing “flashes of light,” noticing “distortion” or loss of vision, and floating objects (floaters) in their vision.
- If the choroidal melanoma is in the front of the eye (near the natural lens), it can push or tilt the natural lens causing an irregular astigmatism resulting in blurring of vision.
- If the choroidal melanoma leaks fluid beneath the retina, that can make the retina detach and cause symptoms of flashing lights and floating specks.
- If the choroidal melanoma is in the macula (center of vision), it can grow beneath the fovea making the patient far-sighted.
- If the choroidal melanoma grows into and destroys the fovea, it can cause visual distortion, loss of vision or changes in color perception.
It is important to note that, in the USA most patients with choroidal melanoma have NO SYMPTOMS AT ALL This is because their tumors are found when they visit their eye doctor for a “routine” eye examination. So everyone should have periodic eye examinations (including dilation of the pupils for ophthalmoscopy).
Other, more unusual presentations of anterior choroidal and iridociliary melanoma are discoloration of the iris, a brown spot on the outside of the eye, an irregularly shaped pupil and glaucoma.
Diagnosis
Choroidal melanoma can be seen by ophthalmoscopy (when your eye doctor looks through a lens into your dilated pupil).
Choroidal melanoma has typical “diagnostic” characteristics that include but are not limited to: pigmentation, thickness, low or moderate internal ultrasound reflectivity, orange pigment on its surface, and leakage of fluid or retinal detachment (on or around the choroidal melanoma).
DR. FINGER HAS DEVELOPED A MNEMONIC DEVICE TO HELP EYE SPECIALISTS DIAGNOSE CHOROIDAL MELANOMA
MOST where Melanoma = Orange pigment lipofuscin + Subretinal fluid + Tthickness*
* (typically >2mm)
 |
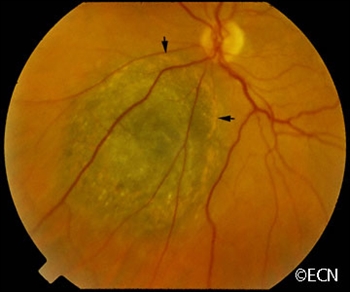 |
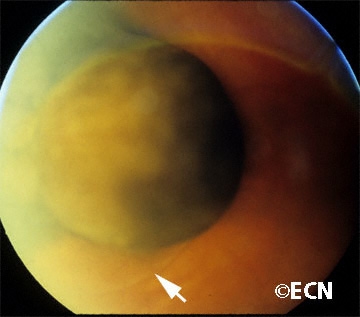
| “Mushroom shaped” choroidal melanoma with a small associated retinal detachment (arrow). | Choroidal melanoma with orange pigment on its surface (arrows). |
| A collar-button shaped choroidal melanoma with orange pigment, subretinal fluid, and thickness greater than 2 mm: all consistent with choroidal melanoma. | A dome-shaped choroidal melanoma with orange pigment, subretinal fluid, and thickness greater than 2 mm: all consistent with choroidal melanoma. |
- Choroidal melanoma pigment is due to naturally occuring melanin that comes from melanocyte cells in the choroidal layer. Choroidal melanoma is usually pigmented. However, they can be variably pigmented and even amelanotic (non-pigmented). Non-pigmented choroidal melanoma is due to a proliferation of melanocytes that have lost their ability to make melanin pigment.
- Orange pigment (lipofuscin) on the choroidal melanoma indicates that cells are dying on the tumor’s surface. The presence of orange pigment is a sign of metabolic activity.
- Ultrasound is typically used to measure the choroidal melanoma size, evaluate internal tumor reflectivity, and look for melanoma extension behind the eye into the orbit (extrascleral extension). Ultrasound shows that most choroidal melanomas are shaped like a dome and less commonly like a mushroom. Ultrasound can also evaluate choroidal melanoma associated retinal detachment.
 |
 |
| Ultrasound of a collar-button shaped Choroidal Melanoma | Ultrasound of a dome-shaped Choroidal Melanoma |
Treatments
Small T1 Choroidal Melanoma:
Patients with a small choroidal melanoma can be treated after their first visit, but since growth helps to prove that the tumor is a cancer, your doctor may suggest “observation” or watching for a small amount of choroidal melanoma growth or change prior to treatment. Your eye cancer specialist should discuss the relative risks and potential benefits of “observation for growth” as compared to “immediate treatment” for choroidal melanoma. Once growth is documented, eye cancer specialists will recommend definitive treatment.
Medium-sized T2 and T3 Choroidal Melanoma:
Around the world, most patients with a medium-sized choroidal melanoma are treated with either radiation therapy or removal of the eye. Though there are several forms of eye and vision-sparing radiation therapy, ophthalmic plaque radiation therapy is the most common and widely used.
Since the results of the Collaborative Ocular Melanoma Study (COMS) suggest that plaque radiation therapy and enucleation of the eye are equally effective for the prevention of metastatic choroidal melanoma, few patients with medium-sized choroidal melanoma are treated by removal of the eye.
In that both enucleation and plaque radiation therapy for choroidal melanoma are likely to harm your vision (in that eye), you should discuss the risks and benefits of these and other treatment options in consultation with your eye cancer specialist.
Large-sized T4 Choroidal Melanoma:
A patient with a very large choroidal melanoma may be treated by removal of the eye (enucleation). This is because the amount of radiation required to destroy a choroidal melanoma that fills most of the eye may be too much for the eye to tolerate.
However, most patients with large-sized choroidal melanoma can be also be treated with eye-sparing radiation therapy. After radiation for large choroidal melanoma, these eyes are at greater risk to have poor vision, to become uncomfortable and may have to be removed.
Additional info
It is important to note that as compared to like-sized malignant melanoma of the skin, patients are much more likely to survive a choroidal melanoma. This is because it is much more difficult for a choroidal melanoma to spread from (get out of) the eye to other parts of the body. However, large (choroidal melanoma) tumor size decreases the chance that vision-sparing treatments will be successful. In general, the larger the choroidal melanoma the worse the prognosis for both vision and metastasis.
Dr Finger suggests you protect your eyes from ultraviolet radiation. He says, “Think of Sunglasses as Sun Block for your Eyes” ™
Patients often ask why they have a choroidal melanoma. Choroidal melanoma is more common among patients with blue vs. brown eyes, those with outdoor occupations and in Australia where there is an ozone hole. Therefore, it seems reasonable to assume (though unproven) that choroidal melanoma is related to sunlight (ultraviolet exposure). In that sunlight exposure has been linked to several eye cancers and diseases of the eye, Dr. Finger suggests that you “Think of Sunglasses as Sun Block for your Eyes” ™ and start wearing your UV blocking sunglasses. They make great gifts too!









